Disease name: Chronic Granulomatous Disease
ICD-10 Disease Code: D71 Functional disorders of polymorphonuclear neutrophils
ICD-10 Disease Group: D70-D77 Other disorders of blood and blood-forming organs
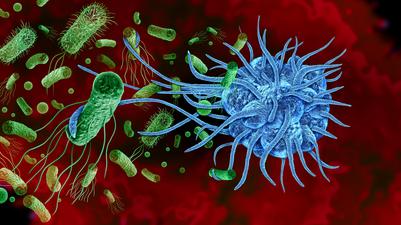
General description:Chronic granulomatous disease (CGD) results in immune system dysfunction, leading to immunodeficiency. This may cause recurring bacterial and fungal infections and inflammation in various parts of the body. Symptoms usually start in childhood, though some may not appear until later in life.
Individuals with CGD often experience serious bacterial or fungal infections every few years; the lungs are the most common site of infection, which often leads to pneumonia. Exposure to certain organic materials can trigger fungal pneumonia. Other areas commonly affected include the skin, liver, and lymph nodes.
In some cases, CGD can lead to autoimmune disorders, where the immune system mistakenly attacks the body's own tissues. Repeated infections and inflammation can shorten life expectancy, but with treatment, most people with CGD can live into their mid- to late adulthood.
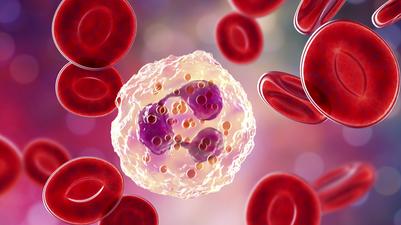
Most cases of CGD are caused by mutations in five genes that each encode a subunit of the NADPH oxidase enzyme complex that plays a crucial role in immune function. The resulting deficiency in the NADPH oxidase enzyme complex leads to decreased production of reactive oxygen species (used by phagocytes to kill bacteria and fungi). Consequently, individuals with CGD are prone to infections and excessive inflammation. Some cases of CGD have unknown genetic causes.
Mutations:CGD is caused by genetic mutations in the CYBA, CYBB, NCF1, NCF2, CYBC1, or NCF4 genes. CGD is categorised into five types, distinguished by the associated genetic variant. A mutation in the CYBB gene (Xp21.1) is found in approximately 65% of cases in North America and Western Europe.
Disease frequency:CGD is estimated to occur in 1 in 200,000 to 250,000 individuals worldwide.
Symptoms:CGD presents with a range of symptoms affecting various organ systems. Common manifestations include severe and recurrent infections, often caused by specific pathogens such as Staphylococcus aureus and Aspergillus spp. Additionally, patients may develop granulomatous lesions, primarily affecting the lungs, lymph nodes, gastrointestinal tract, and liver. Up to half of patients may experience symptoms such as diarrhoea, abdominal pain, and failure to thrive. Common complications can include pneumonia, abscesses, cellulitis, adenitis, and osteomyelitis. Mycobacterial diseases are typically limited to tuberculosis or disseminated Bacillus Calmette-Guérin (BCG) infections, while invasive fungal infections are frequent. Dysregulated inflammation and granuloma formation can lead to various complications, including chorioretinal lesions, gastric outlet obstruction, inflammatory bowel disease (IBD), and wound complications. Most female carriers of CGD show no symptoms unless a significant portion of their neutrophils are dysfunctional. Some individuals with CGD may develop autoimmune disorders such as discoid lupus erythematosus and antiphospholipid syndrome.
Treatment:Antibacterial and antifungal prophylaxis can be used to prevent infections in CGD. Recommended treatments include lifelong daily doses of trimethoprim-sulfamethoxazole (antibacterial) and itraconazole (antifungal). Interferon-gamma, administered three times weekly, is also advised. Haematopoietic stem cell transplantation is a potentially curative option that is gaining utilisation. Some gene therapies to address the causative mutation have shown promise. Granulocyte transfusions may be employed in severe infection cases.
Sources:- https://www.icd10data.com/
- https://www.orpha.net/consor/cgi-bin/index.php
- https://rarediseases.org/
- https://medlineplus.gov/genetics/
- https://www.cdc.gov/