CAR-T cells: a Shift in Cancer Immunotherapy
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
Welcome back to WeDoCRISPR, this is going to be a special one!
In the previous episodes, we mentioned the use of Chimeric Antigen Receptor (CAR) T cells to fight cancer. We realize that we never spoke about this topic before and we don’t want to leave any loose ends around here, so for all the geeks curious about this topic or those who may even be studying about it at this very moment, this episode is for you!
Antigen presentation is the key to how our immune system works
Among all the complex systems that make sure we keep going, the immune system is the one that we take notice of when it snaps into action! When your body is invaded by infectious agents like viruses and bacteria, you are quite aware of the rising temperature coming from your fever, as well as less pleasant countermeasures like vomit or “else”.
This is your immune system turning your body into the worst Airbnb experience imaginable for those pesky infectious agents! While you crawl under your blanket and force your cat into becoming a living warm bag – giving it nightmares that will last for 3 of its 9 lives – there is an ongoing battle in your body.
Here, we got spotters called antigen-presenting cells (APCs), which will find and expose in their surface “traces” of the foreign agent. This is what we will call an “antigen”, a piece of protein from a foreign agent that can be recognized by other immune cells. These spotters - together with the precious support of the heralds, the helper T cells – then unleash the hounds, the cytotoxic T cells.
This army of fierce warriors is deployed when their receptors recognize the foreign antigen, activating them. At the end of the battle, once they’ve defeated the enemy, some of these T cells will hold a grudge forever, and always remember who dared to attack their kingdom. Those cells, called memory cells, will be able to quickly activate a blitzkrieg-type attack if the same enemy ever dares come back.
Yes, we are their little princess.

This is pretty much what we all know about the immune system. And if you didn’t, you’re welcome! What some of us may not be aware of is that our immune cells are very inclusive, and they treat – and threaten – everyone the same. This includes cancer.
Cancer immunotherapy: turning T cells into bounty hunters
T cells can not only kill external pathogens, they are also able to kill cancer cells. However, cancer cells are great at making it really difficult to kill them. This can be due to several reasons, but the main one is that cancer cells “blend” in with our cells. Since they are cells from our own body, on their surface, they expose antigens that are not recognized as “foreign”, and therefore no real immune response is triggered. Another reason is that your T cells are not strong enough to kill all cancer cells, particularly if there are a lot of them, so we need to bring some backup!

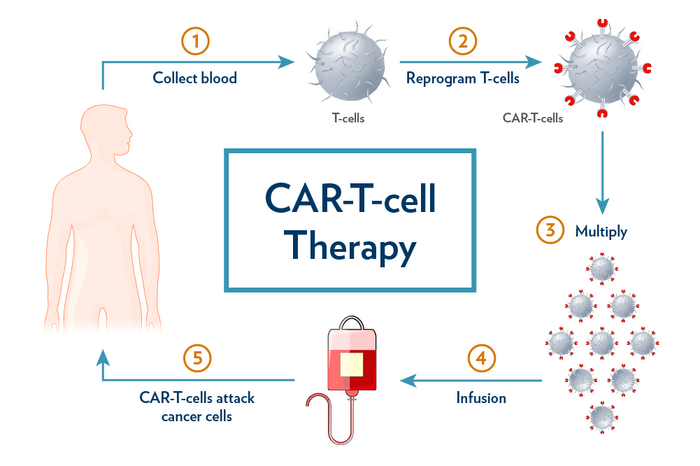
This is where cancer immunotherapy comes in! Chimeric Antigen Receptor (CAR) T cells is a concept born at Penn University under the lead of Dr. Carl June, which aims to equip the T cells with a synthetic receptor. This receptor mimics the essential portions of the ones occurring in nature but is designed to recognize an antigen of choice found exclusively in cancerous cells. This allows us to super-power CAR-T cells so that they're way more efficient at detecting and eliminating those pesky cancer cells.

CAR T cells can cure blood cancer
One of the setups in which CAR T cells have scored the highest rate of treatment success is for blood cancer: leukemia, lymphoma, and multiple myeloma.
In this case, the antigen of choice is CD19, a surface protein that is over-expressed in leukemic B cells. However, our T cells are normally incapable of recognizing CD19. That’s because, during the development of the immune system, any T cells with receptors that recognize “self” antigens are eliminated in the thymus to guarantee that they won’t attack our own body. And yes, CD19 is not unique to leukemic cells but also present in differentiated, non-cancerogenic B cells.
So why would we use CAR T cells that recognize CD19? Won’t they attack our healthy B cells?
Indeed, patients undergoing CD19 CAR T cell therapy experience an overall reduction in their B cell count, or B cell aplasia. This is actually an indicator of how well the therapy is working! The more B cell aplasia, the better! Because for any healthy B cell eliminated, so many more leukemic B cells will be gone.
Regardless, immunoglobulin replacement is now a standard of care to manage B cell aplasia following this kind of therapy.
To this day, CAR T-based therapies have shown an encouraging rate of success, with around 50% of patients being cancer-free long after receiving treatment. Isn’t that amazing? These therapies are approved and on the market for blood cancer: Kymriah™ (tisagenlecleucel); Yescarta™ (axicabtagene ciloleucel), Tecartus™ (brexucabtagene autoleucel), Breyanzi® (lisocabtagene maraleucel) Abecma® (idecabtagene vicleucel)
This sounds awesome, and it is. However, if you follow us from the beginning you know that there is a “but” coming your way. Indeed, CAR T cell manufacturing is not always as easy as it sounds. On the one hand, CAR T cell manufacturing has some bottlenecks that may render it difficult to get them to the patient in due time. On the other hand, cancer cells have many ways to defend themselves and evade the immunosurveillance of our body, even escaping CAR Ts!
And this is where gene editing and CRISPR engineering come in to, once again, save the day!
In the next episode, we will tell you how to make a powerful cancer therapeutic like CAR-T even better with CRISPR! Don’t miss it!
To get more CRISPR Medicine News delivered to your inbox, sign up to the free weekly CMN Newsletter here.
Tags
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.