Clinical Trial Update – CRISPR-Based Diagnostics for Infectious Disease
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
When CRISPR-Cas9 was first exploited as a targeted gene-editing tool in 2012, researchers quickly saw its huge potential for novel gene-editing therapies. Today, there are many CRISPR-based therapies in clinical development for cancer, blood diseases and inherited single-gene disorders.
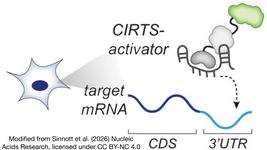
As the CRISPR field advanced and other Cas endonucleases were discovered, e.g., Cas12 and Cas13, it became clear that the search function of CRISPR could also be used to seek out and detect specific nucleic acid sequences, opening up huge opportunities for new and highly sensitive diagnostics. The COVID-19 pandemic has been a catalyst for many new CRISPR-based diagnostic strategies, many of which we have covered in recent months.
CRISPR-Based Diagnostics for Infectious Disease
Recently, the Children's Hospital of Fudan University in China announced two clinical trials to evaluate the potential of CRISPR-Cas to diagnose infectious diseases in children. The first trial evaluated CRISPR-based detection of certain enteroviral serotypes, while the second will evaluate CRISPR-based detection of pathogenic Bordetella species and resistance genes to the antibiotic erythromycin in a single step.
Clinical Trial for CRISPR-Based Enteroviral Detection
Enteroviruses are RNA viruses from the Picoronavirus family. There are at least 70 distinct human serotypes that cause a broad range of conditions that occur along a continuum from mild, e.g., childhood rashes to severe, e.g., polio.
Enteroviruses are shed in respiratory secretions and stool and are sometimes present in the blood and cerebrospinal fluid (CSF) of infected patients. Diagnosis is usually made following a clinical evaluation that is sometimes supported by viral culture and reverse transcriptase–polymerase chain reaction (RT-PCR)-based detection. Other diagnostic approaches include imaging, antibody testing, and analysis of whole blood cell counts in CSF. Laboratory diagnosis is usually unnecessary in mild cases but it becomes highly relevant in severe cases to guide treatment as well as curb potential serious outbreaks. Most medical facilities have the means to determine whether or not an individual is infected but there is currently no single test that can discriminate between the different serotypes.
The observational trial, led by Liling Qian at Children's Hospital of Fudan University, evaluated the potential of a CRISPR-based detection system to detect and discriminate between different enteroviral serotypes. A CRISPR-based testing platform was developed and evaluated using the remainders of samples of stool, blood and CSF from 500 children up to 18 years of age with suspected or confirmed enterovirus infection. Patients with a clinical diagnosis of non-enterovirus infection were excluded from the study. The detection platform was compared to real-time PCR or conventional PCR for its ability to detect enterovirus, its discriminatory power, its sensitivity, which was deemed to be 90 %, and its specificity, which was deemed to be 95 %.
Clinical Trial for Rapid CRISPR-Based Bordetella Detection
The second trial is for a new CRISPR-based detection platform for Bordetella, the bacterial genus responsible for pertussis or whooping cough. Pertussis is an acute respiratory infectious disease caused by Bordetella pertussis, and although the disease is vaccine-preventable, outbreaks and epidemics occur from time to time. Infection with three other bacterial species, Bordetella parapertussis, Bordetella bronchiseptica, and Bordetella hosei can lead to pertussis-like conditions with symptoms that overlap with whooping cough.
The current diagnostic approach to Bordetella infection includes culture (although this is difficult), Bordetella pertussis specific antibody (PT-IgG) detection in serum, and PCR-based Bordetella pertussis nucleic acid detection. Challenges in diagnosis stem from the fact that it is clinically difficult to distinguish between pathogenic isolates, and none of the available diagnostic tools are suitable for early diagnosis.
The new study, which is led by study director Chuanqing Wang, PhD at Children's Hospital of Fudan University is prospective, meaning that it will address the usefulness of a new CRISPR-based detection platform by testing incoming samples that meet the study’s inclusion criteria over time. The new platform deploys cross-priming amplification (CPA), which is a type of isothermal nucleic acid amplification, in conjunction with CRISPR-Cas technology and has the potential to discriminate between the 4 pathogenic Bordetella species as well as detect point mutations in erythromycin resistance genes in a single step. The new platform will be compared to Bordetella pertussis culture and identification methods.
Research subjects will include 600 children up to the age of 18 years, with clinical symptoms of pertussis whose symptoms don’t resolve following treatment with cephalosporin antibiotics. The study aims to enroll 600 individuals with clinically suspected pertussis from whom nasopharyngeal swabs have been taken within the period from October 2021 to June 2022.
You can find the available details on the Enterovirus and Bordetella trials in our clinicals trials database. We have contacted the study directors to find out more about the CRISPR-based detection methods used in these trials as well as future plans. We will update with more details when possible.
Tags
ArticleDiagnosticsDiseaseBordetella PertussisEnterovirusesCRISPR-CasTrials
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.