Real World Applications
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
Before we start, as we write a lot of scientists, clinicians and patients are celebrating the approval in the UK of Casgevy on Thursday 16 November 2023. Mark this date, as this is the first CRISPR/Cas-based therapy to be approved beyond a restricted number of patients involved in clinical trials.
The timing could not be perfect since today's article will be about real-world examples of CRISPR applications in human clinical trials!
So let's jump into it!
We do realize that the last article was quite challenging both to write and to read due to the great amount of information and technicalities it was packing.
This article won’t be any shorter, but it will give us all a breather by focusing on the application of CRISPR in current clinical trials. The fun stuff!
Read this line again, because its meaning is broader and more powerful than what you realize:
i) CRISPR is already being deployed in humans to tackle genetic diseases and other disorders. And Casgevy is a prime example of it!
ii) By reading our last five articles you already have a good understanding of how CRISPR works, and this is a technology that can be directly applied to a clinical scenario.
And there is more to it. So far, we just introduced you to how CRISPR can be used to Knock-Out a gene. This is quite a simple and straightforward thing to do and yet it is powerful enough to change the life of a patient.
And today, we are here to see how!
For now, we will focus on the application of CRISPR to monogenic disorders, meaning conditions associated with “just” one faulty gene. While CRISPR can also be used to target more than one gene at a time – a practice named multiplexing – this requires other considerations that we have not covered yet, so we will get into it once we’re more advanced in our discovery of CRISPR.
Before moving to the actual clinical trials, let’s first ask ourselves how shutting a gene down can be beneficial for a patient. While the canonical type of mutation you’ve probably heard about is that which causes a gene to stop working, those are not the only mutations that can cause a disease. Indeed, there are other mutations that don’t stop protein production but can alter it in ways that can cause serious problems in our cells. This can be because the protein gains a detrimental new function, or because the protein folds incorrectly and accumulates in the cell, for example.
In those cases, turning a malfunctioning gene off can eliminate this effect and ameliorate or completely cure a condition.
Using gene KO to treat transthyretin amyloidosis
An example of a condition caused by a malfunctioning gene is Transthyretin amyloidosis shortened as ATTR amyloidosis. This is quite a nasty disease, where misfolded amyloid fibrils accumulate in organs and peripheral nerves causing fatigue, abdominal swelling, breathing difficulties, and arrhythmia. Standard medical care can somehow try to reduce the accumulation of misfolded fibrils but cannot stop it. This is where CRISPR/Cas9 comes in.
Intellia Therapeutics devised a strategy aiming at KO the TTR gene in the liver– where most of the corresponding TTR protein is synthesized – to block the production of these fibrils. This can be done because TTR normal function is not essential, and if the TTR protein is absent -rather than mutated -, that is not nearly as deadly as the ATTR amyloidosis.
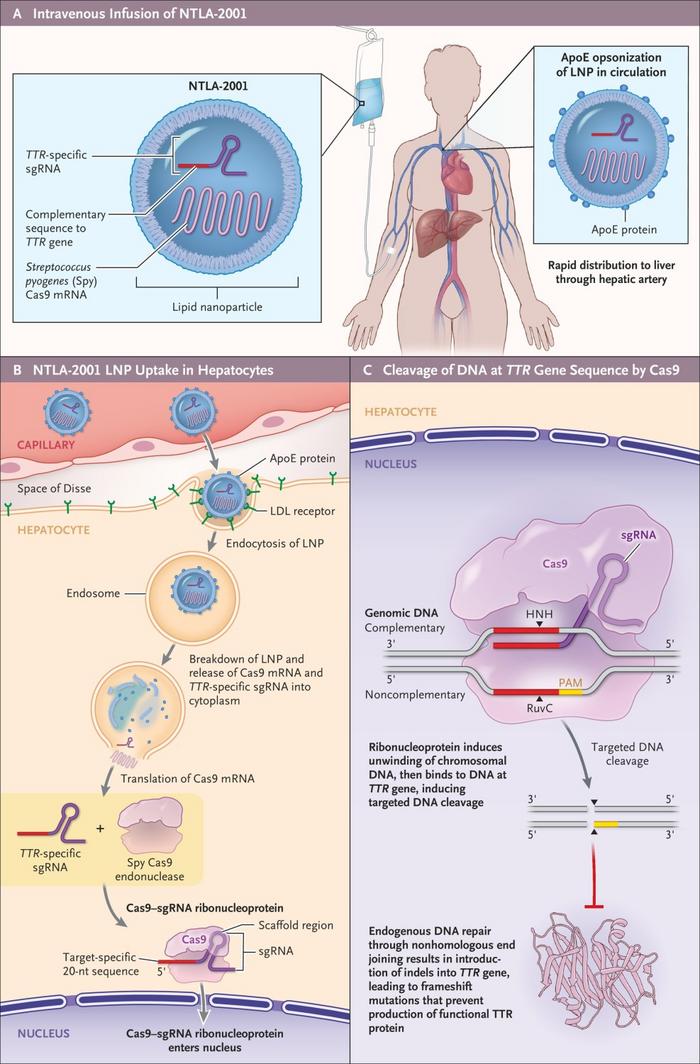
In this clinical trial, dubbed NTLA-2001, it was possible to reach more than 80% of TTR protein reduction, which was accompanied by a decrease in the accumulation of misfolded amyloid fibrils, the leading cause of the disease! The results were so encouraging and promising that now the clinical trial is in phase III, meaning that the strategy is being tested on a broader number of patients!
While this is already fascinating, we hear you craving for more examples of how a double-stranded break (DSB) can be leveraged to develop a cure. And we will deliver.
What about disrupting a genetic region to reactivate a previously silent gene?
Treating beta-thalassemia and sickle-cell disease by reactivating fetal hemoglobin
What may sound like witchery is instead a quite elegant approach that was undertaken to treat both transfusion-dependent beta-Thalassemia and Sickle-Cell-Disease (SCD). Both conditions are characterized by mutations in the HBB gene, which codifies the beta-subunit required for the formation of adult hemoglobin, the protein responsible for carrying oxygen in our red blood cells. In these two conditions, mutations of the HBB gene can either lead to a misshaped adult-hemoglobin – Sickle-Cell-Disease – or decreased/ absent levels (beta-Thalassemia) of it. Affected patients experience hemolysis, anemia, painful vaso-occlusive episodes, irreversible end-organ damage, and a reduced life expectancy. The current line of treatment includes regular blood transfusion, and the only definitive treatment is hematopoietic stem cell (HSCs) transplantation, a practice per se not devoid of risks and limited by compatible donor availability.
So how do we solve this with CRISPR? In this case, knocking out the mutated HBB won’t do much. However, to crack this particular nut, we have to remember that in our genome we still hold the information for the fetal subunit of the hemoglobin. Fetal hemoglobin is the type of hemoglobin that is found in our blood while we’re still in the womb, and it binds oxygen stronger than normal hemoglobin. This helps us get oxygen from our mom’s blood. After we’re born, the fetal hemoglobin gene is turned off and we use the regular one. Although it is off, the fetal hemoglobin gene is still there and may be used to compensate for the lack of the adult one. Even better, as the fetal hemoglobin has a higher affinity for oxygen compared to the adult one, even lower levels may actually be helpful.
This was the reasoning pursued by the team of CRISPR Therapeutics. And how did they manage to turn it back on? Well, here it comes the elegant part of the matter: they aimed to disrupt the region driving the expression of BCL11A, a transcription factor that is involved in keeping the fetal hemoglobin switched off.
Wait? Why not simply knock out BCL11A as Intellia did with TTR? Well, that’s because a transcription factor normally has more than one target, so knocking out BCL11A would likely create far worse problems. Instead, by disrupting a regulatory region that drives BCL11A expression only in red blood cells, they could preserve its function in other cells.
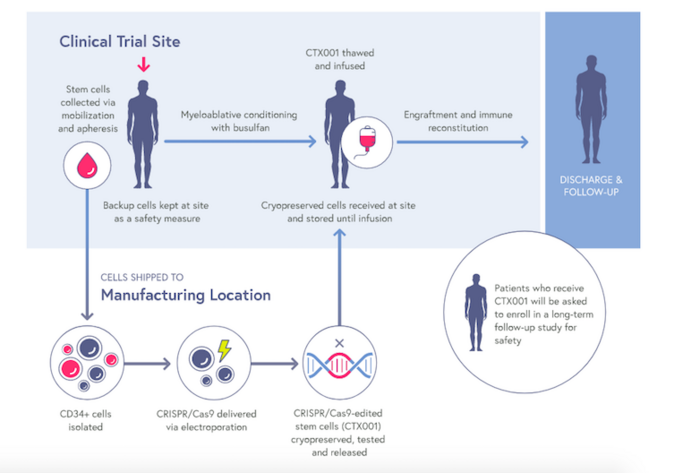
Hey, we didn’t say that CRISPR approaches were always simple. We cannot always just kick down doors, after all, this is still engineering. This strategy paid off. In fact, HSCs derived from sickle-cell disease and beta-thalassemia patients and treated with CRISPR showed clinically relevant levels of fetal hemoglobin, and all the treated patients are currently free of the need for blood transfusions, marking a striking step for CRISPR into clinical trials.
The results achieved made it possible for this approach to be the first worldwide CRISPR-based therapeutic to be approved in the UK with the name of Casgevy!
Removing the HIV virus from our cells
We saw an example of how CRISPR it is being used to cure a condition by eliminating the function of a defective gene and, in another case, how it can be indirectly used to reactivate the function an inactive gene. For our next and last trick, we are going to show you how CRISPR can also be used to remove an entire infectious viral genome from patient’s cells. We know that at the very beginning, we said we would only talk about monogenic disease. However, this approach is so cool and so relevant today that we cannot wait any longer!
We are talking about eradicating the HIV virus, the leading cause of Acquired Immunodeficiency Syndrome (AIDS). This disease has been very relevant in our society for the last decades. The standard of care right now is antiretroviral therapy (ART), which can “control” the virus infecting the patients’ cells and reduce its effects, allowing patients to live a pretty normal life. However, the patients need to take medications for their entire life, with the potential side effects that come with them like diarrhea, fatigue, headache, liver problems, nausea, stomach pain, vomiting, and poor appetite.
The reason why the HIV virus is so infectious and difficult to eliminate is that once it enters the cells it sticks to them permanently. Oh yes, that small little rat retrotranscribes its RNA genome – HIV is a ribo virus – into DNA and it integrates it into our genome.
Can you believe that?
From this point, the virus can hijack the replicative system of our own cells to replicate itself and mess up our immune system.
“Well, not in my backyard!” this is probably what really went through the mind of the scientists at Excision Biotherapeutics when they squeezed their brains out to find a potential solution to liberate patients from HIV.
And it looks like they did!
See, when the HIV virus integrates into the genome, it leaves a distinct footprint in the form of long-terminal-repeats (LTRs) at the two ends of its DNA sequence. So, what would happen if we could make CRISPR/Cas cut at the two ends of these LTRs? Exactly, the HIV genome would be cut out of the patient’s DNA.
But wait? Could the sequence not just flip over and come back into the genome?
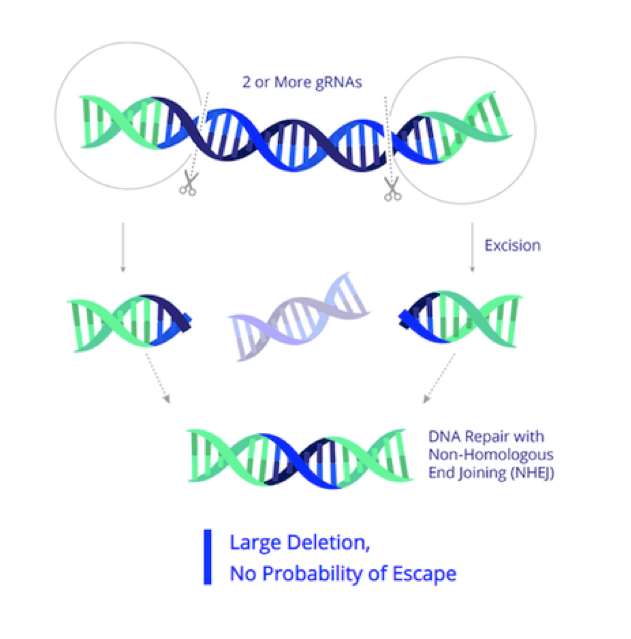
This is a legitimate question and that’s why the strategy included not only a sgRNA targeting the LTRs, but also an extra sgRNA targeting the Gag gene which it is crucial for the virus particle assembly. By doing this, they made sure that once cut out, the virus genome stays out and nonfunctional. Following-up on previous successful studies in monkeys, patients infected with HIV were administered intravenously with CRISPR/Cas encapsulated in a viral vector. The latest report from Excission BioTherapeutics reported encouraging interim results of EBT101 meaning that the treatment was well tolerated and CRISPR could be detected in the patients’ bodies. Hopefully we will hear from them soon and we learn whether the HIV virus was eradicated too!
This brings us to the end of this article. These are only a few examples, and a lot more it is going on behind the scenes. If you want to learn more, you can jump to the clinical trial section of CRISPR Medicine News and why not even witness the change in first person by attending the upcoming CRISPR Medicine Conference in Copenhagen on April 2024!
Before we close, of course, we need to tease you with what is coming next. Everybody likes a bit of a cliffhanger every now and then!
In the next episode, we will introduce you to the “ugly” side of CRISPR/Cas, the off-targets!
Take your time to digest what we learned so far and get ready for the next episode.
Enjoy your weekend, share, comment, like.
And as always, we will see you in the next one!
To get more CRISPR Medicine News delivered to your inbox, sign up to the free weekly CMN Newsletter here.
Tags
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.







