CRISPR Face Mask Can Detect COVID-19 And Other Pathogens
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
A team of intrepid scientists has made the bold decision to take CRISPR out of the gene therapy clinic and bring it into the garment industry instead.
The researchers, led by Peter Nguyen and James Collins from Harvard University's Wyss Institute for Biologically Inspired Engineering, have developed a shelf-stable biosensor made of freeze-dried synthetic circuits loaded up with CRISPR enzymes. After they embedded those sensors into garments, armbands, and even face masks, the team found that they could detect specific pathogens or other molecular targets at extremely-low concentrations, according to research published Monday in the journal Nature Biotechnology.
The project builds on decades of synthetic biology research that the researchers say has been stuck sequestered away inside the lab and had limited practical use but is now surging into relevance. One particularly timely aspect of their work is a new prototype face mask that, thanks to embedded CRISPR sensors, can detect a COVID-19 infection with the same level of precision as a quantitative PCR test, the current gold standard for coronavirus testing. Not only is that potentially a valuable tool in the fight against the coronavirus pandemic, but it could revolutionize the market of wearables, which are right now limited in terms of what kinds of data they can collect.
»One thing that [current wearables] can't do, since they probe physiological signals through optical or electrical means, they can't run chemical reactions. I think that's the next big frontier. Imagine having a device that you wear that can run chemical analyses of your environment or what you're exposed to. That opens up a whole new field for wearables. You're no longer constrained to simple physiological signals from the body; you could probe anything you're exposed to. These sensors can tell you that you were just exposed to this bacterium or that virus down to the nucleotide level. It opens the field to detecting any living thing that you were exposed to,« says microbiologist and cellular device researcher Peter Nguyen, who's the lead author of the new paper.
»Any metabolites, any toxins, any nerve agents, we can detect that as well. We think this is the first demonstration that opens this huge box of tools that we can use for robust wearables,« he adds.
Detecting specific genetic sequences
The idea is to use all the molecular machinery that's usually inside a specially engineered cell. But the researchers lyse the cell to take all the proteins and enzymes out and use them as components in a cell-free circuit embedded or woven into a textile rather than treating the cell as a standalone machine.
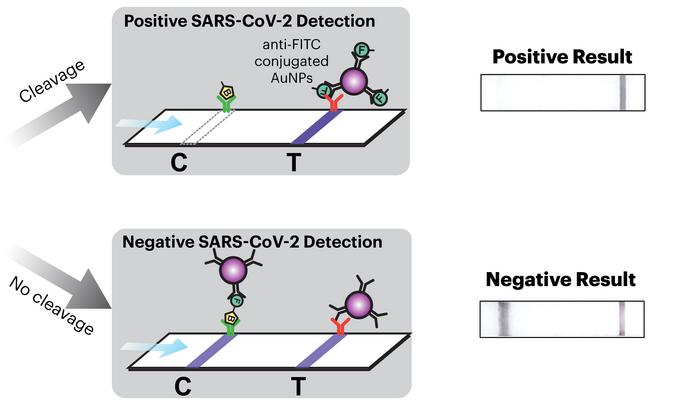
To detect specific pathogens or other molecular targets, the researchers used CRISPR-Cas enzymes — Cas13a for RNA detection and Cas12a for DNA — and programmed them by integrating guide RNAs (gRNAs). The Cas12a- or Cas13a-gRNA complexes then pick up on the specific genetic sequences of their particular target and, depending on the specific case, produce a fluorescent or colourimetric readout when they detect contamination.
Whether you want the wearable to detect COVID-19 or Staphylococcus aureus, the only part of the circuit that needs to change from one test to another is the specific gRNA sequence that tells the CRISPR-Cas enzyme what to look for.
»You drop in the gRNA, and you switch the sensor from detecting one thing to another. The way it's implemented on our prototype wearables is that you would have to wear the wearables designed to detect a very particular thing. They would already have to have a gRNA inside of them,« says Nguyen.
Freeze-dried CRISPR - just add water
Until this research, biological systems haven't been integrated into wearables or clothing for one unavoidable reason: they tend to die off without food, water, and waste management. The Wyss Institute researchers needed a way to make their technology shelf-stable in a way that proteins, enzymes, and other biomolecules typically aren't upon being taken out of the cell. What they realized, however, was that their synthetic circuits could survive being freeze-dried into a powder and rehydrated whenever it's time to use them. And once it is time, all of the reactions can then occur at room temperature. These powders containing all the machinery for each stage of reaction, embedded into flexible materials, could live on a shelf as long as a year, Nguyen says.
»You can store that powder on a shelf because it's freeze-dried like a pack of ramen or a pack of instant coffee. All you have to do is just add water. This is the shocking part, and many people don't believe us when we tell them that all you have to do is add water, and the circuits will rehydrate, and they'll work after they've been sitting on a shelf for several months. Anywhere from six months to a year,« Nguyen says.
» That's a huge difference,« he adds.
Once they had the technology in hand, Nguyen says, he and others in Collins' lab brought their freeze-dried circuits to the world in gradual stages. First, they developed a rapid test for Ebola, then vaccines.
»We then developed biomanufacturing so we could make the vaccine on-site using freeze-dried reactions. All you had to do is add in the DNA and water and wait, and you make a vaccine or a therapeutic on-site. That was also pretty amazing for us,« Nguyen says.
From there, they developed freeze-dried educational kits for students — like an equivalent to those classic chemistry sets but for conducting biological and even CRISPR reactions — that are currently sold to American high schools under the BioBits brand.

»We wondered how far we could push this. That led us to wearables because wearables technology has to be really, really robust. It has to be integrated into clothing, and it has to work relatively autonomously. It has to just work,« says Nguyen.
»To do that using synthetic biology is a tall order. We wanted to put the bar very high and see how far we could push it. It worked beautifully,« he adds.
Detecting one viral particle per millilitre
As it stands right now, the prototype wearables take two forms. One resembles the more conventional notion of a wearable: an armband, a garment, theoretically even personal protective equipment, PPE, with freeze-dried circuits integrated into it.
»For the wearables themselves, we wanted to develop a system that was as sensitive as possible. We designed it so we could use fluorescents as an output. For example, we made a jacket that has fiber optics integrated into the fabric. So the fiber optics transmit the light from an activated sensor to a small detector that you would wear on your belt. Or it can be weaved into or integrated into the jacket,« Peter Nguyen says.
Using laboratory equipment rather than garments, Nguyen found that they could detect pathogens at a concentration of one viral particle per millilitre of the sample, a level of precision that far exceeds anything currently in use for COVID-19. And moving those reactions from high-quality lab equipment to wearables gives fluorescent readouts from the garments at nearly the same level.
It's in this situation where the CRISPR sensors excel.
»A lot of people don't realize that CRISPR can be used for detection. If you think about it, that is the original function of CRISPR in bacterial cells: to detect whether or not they're being infected. It's incredible at that function. We're going back to what the original function of the system is and reusing it for our purposes,« says Nguyen.
For now, the wearable would need to be designed to detect a single, specific biohazard. The gRNA used to program the CRISPR-Cas sensors can easily be swapped out, Nguyen says, but so far, there's no way to use the new system to test for multiple pathogens at once. At least not in a way that would differentiate between them.
The issue is that every positive signal would look the same in the fluorescent output, so someone wearing a device with multiple gRNAs would only know that they were exposed to something without being able to determine what it was. That could make it a valuable tool for a healthcare worker fighting an outbreak in a field hospital, for example, because they already know what they're likely to encounter. But it also makes the wearable less useful as a generalizable consumer gadget for the health-conscious public.
»There's no diagnostic test right now that [detects multiple biohazards] using CRISPR. That's something that we're working on. Baby steps — the first thing was just getting this to work in wearables at all,« says Nguyen.
COVID-19 face mask
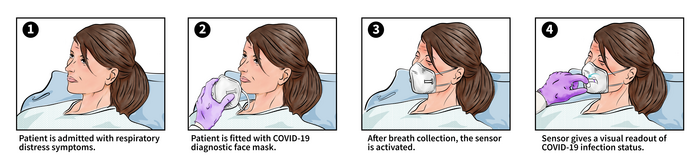
And then there's the face mask with a built-in COVID-19 test. The test is slightly less sensitive to pathogens than the other wearables, but that's because the team decided to prioritize user-friendliness and simplicity over laboratory-grade precision.
The mask works first and foremost as a way to gather up aerosolized samples into a contained area. A sensor pad located right over the mouth and nose inside the mask collects whatever particles the person might be exhaling. It takes about 15 minutes to breathe out a good enough sample — Nguyen suggests 30 minutes just to be sure — and then a single button rehydrates and reactivates all of the biological machinery, triggering a series of reactions that all take place on that same sensor pad.
»We have a lysis reaction that breaks apart the virus, and then we have an amplification reaction. We have nucleic acid amplification that converts things from RNA to DNA. Then you have the CRISPR reaction that detects if that signal is there, then it gets translated to the lateral flow assay for the output. All these reactions happen at room temperature,« Nguyen says.
Between an hour and 90 minutes later, the mask provides a positive or negative readout that looks similar to the single or double bands of an over-the-counter pregnancy test.
The mask is less accurate than the jacket, but that's by design, Nguyen explains.
»When we integrated [the circuitry] into the face mask, we knew it would take a hit. To make it work in a robust wearable format, you have to sacrifice a lot. But we were lucky in that the hit [in precision] we took still put us right in the realm of RT-PCR. If you take a nasal swab and send it to the lab for a World Health Organization RT-PCR test, it'll be as sensitive as the face masks that we have right now,« he says.
»The sensitivity, this is where the CRISPR detection technology truly shines. We can easily distinguish between COVID-19 and all of the different coronavirus strains circulating out there. We should be able to quickly adapt this for the variants that are emerging right now, which is something on our radar that we need to address and develop these face masks for,« Nguyen says.
He added that the lab is also working on a mask that could test for each SARS-CoV-2 variant simultaneously and specify which one it detects.
Future diagnostic
Nguyen, Collins, and the rest of the team have been talking with various companies about mass-producing a face mask embedded with their modular, freeze-dried COVID-19 test since December 2020, when they finished testing the mask for this new paper. Nguyen says they've had productive conversations, but they're still open to talks with any other companies that might be interested in taking the project on. Right now, each prototype is hand-built in the lab but still, discounting the cost of a store-bought mask only costs about five US dollars. That said, Nguyen says that he expects the face masks to get even cheaper and the reactions to get even faster once they partner up with a company and figure out manufacturing.
Nguyen envisions a future where anyone could head to their pharmacy and grab a face mask that will serve as a disposable, protective, and point-of-care diagnostic device. Someday, the masks could not only protect the wearer and the people around them, but also warn them when they've been exposed to the coronavirus, a particularly rough seasonal flu, or whatever the respiratory disease du jour happens to be — so that they not only know to get treatment but also precisely what it is they should be treated for.
»No one in the lab wants this to end up as an academic exercise that you see as a footnote in a paper somewhere. We want it to be out there, on the shelves, for anyone to buy,« Nguyen says.
Link to original article in Nature Biotechnology: Wearable materials with embedded synthetic biology sensors for biomolecule detection.
Dan Robitzski is a science journalist and former neuroscientist based in Los Angeles.
Video from the team at the Wyss Institute:
Wearable Synthetic Biology - Clothing that can detect pathogens and toxins.
Credit: Wyss Institute at Harvard University
Tags
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.