Non-viral CRISPR Therapy Alleviates Symptoms in Humanised Mouse Model of Primary Hyperoxaluria Type 1
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
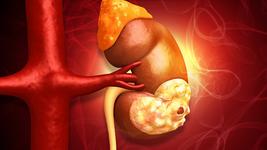
Primary hyperoxaluria type 1 (PH1) is a rare and potentially life-threatening genetic disorder that arises through mutations in the AGXT gene. This results in deficiency or dysfunction of the enzyme alanine-glyoxylate aminotransferase, which leads to a harmful accumulation of oxalate in the kidney and other organs. PH1 typically debuts in early childhood and affects approx. 45,000 people worldwide.
Recently, two small interfering RNA therapies, marketed as Oxlumo (US, EU) and Rivfloza (US) have emerged for PH1. These work as substrate reduction therapies (SRT) by targeting the transcripts for specific enzymes in the oxalate biosynthetic pathway, thereby reducing key substrates required for oxalate production. While these offer much-needed treatment options for PH1 patients, multiple doses are needed to maintain their therapeutic effect, while CRISPR-Cas9-based SRT therapies delivered by adeno-associated virus (AAV) have raised safety concerns.
Now, scientists at Shanghai Frontiers Science Center of Genome Editing and Cell Therapy and YolTech Therapeutics report pre-clinical data to support a non-viral gene-editing approach for PH1 based on SRT, that led to lasting effects in mice, without significant side effects.
Non-viral CRISPR therapy reduces oxalate levels in PH1 mice
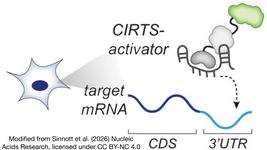
The team first generated a mouse model of PH1 using lipid nanoparticles (LNPs) to intravenously deliver Cas9 mRNA and a highly-efficient and specific single-guide RNA designed to target the AGXT gene. They found that this model exhibited a PH1 phenotype characterised by elevated oxalate excretion and calcium deposition in the kidney after drinking a solution of ethylene glycol (which served as a substrate for oxalate formation). No significant off-target editing was observed in the liver of PH1 mice, following deep sequencing of 30 potential off-target sites of the selected gRNA.
Two weeks after the PH1 mice were generated, they were treated with a single intravenous dose of LNP-CRISPR-Cas9 and a gRNA targeting the mouse Hao1 gene (mHao1). This gene encodes hepatic glycolate oxidase (GO), an enzyme that converts glycolate to glyoxylate. Two weeks later, the mice were sacrificed and AGXT and Hao1 editing efficiencies were assessed through deep sequencing. This revealed that AGXT expression was almost silenced while 61-75 % editing efficiencies were observed for Hao1 in liver tissue.
With respect to PH1 phenotypes, the team observed reduced glycolate oxidase expression and reduced urinary oxalate levels that continued over a 12-month follow-up period. Long-term editing efficiency of AGXT and Hao1 was also confirmed at 12 months post-treatment, and gene editing of Hao1 was corroborated with western blot and immunohistochemistry that indicated reduced GO expression in PH1 mice compared to control animals.
The therapy also works in a humanised mouse model of PH1
To facilitate clinical translation of the new therapeutic approach, the researchers generated a humanised Hao1 mouse model, whereby a modified human Hao1 sequence was injected into mouse zygotes to generate hHAO1 KI mice. The resulting transcript was detected in the livers of hHAO1 KI mice but not in their control littermates, which exhibited mHao1 expression. Those findings suggest that hHao1 expression in the knockin mice mimics Hao1 expression in humans, which may offer a useful system for future studies of human Hao1 expression.
Intravenous delivery of LNP-CRISPR-Cas9 and a gRNA targeting hHao1 in the knockin mice demonstrated dose-dependent in vivo editing efficiency of hHao1 (highest efficiency 59%), reduced or absent hHao1 gene and protein expression, and reduced urinary oxalate levels.
The findings demonstrate that LNP-mediated in vivo delivery of a CRISPR therapy can safely alleviate PH1 symptoms in mice that express human Hao1. YolTech Therapeutics is now advancing this approach through the clinic, with an ongoing clinical trial of YOLT-203. You can read more about that in our latest clinical trial update here.
The findings were published last week in Molecular Therapy (1).
References:
1. Jiang Y, Chen S, Hsiao S, Zhang H, Xie D, Wang ZJ, Ren W, Liu M, Liao J, Wu Y. Efficient and Safe In Vivo Treatment of Primary Hyperoxaluria Type 1 via LNP-CRISPR/Cas9-mediated glycolate oxidase disruption. Mol Ther. 2024. Oct 8:S1525-0016(24)00663-4.
Tags
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.