A Gene-Edited Cell Therapy for an Incurable Disease: Researchers Receive USD 4.8M Grant to Treat Friedreich’s Ataxia
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
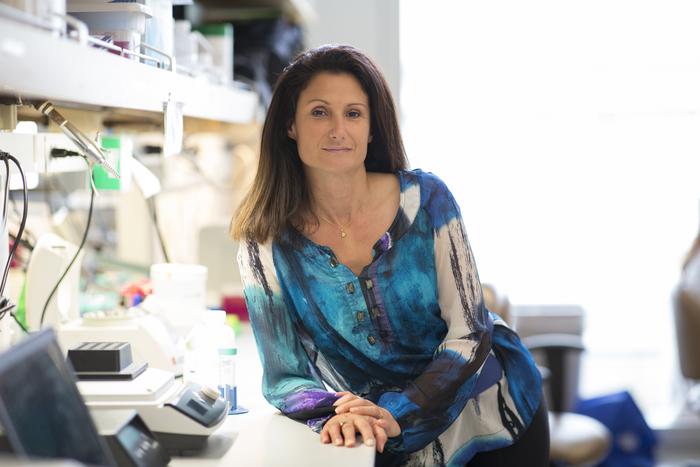
From the beginning of her scientific studies, Professor Stephanie Cherqui of UCSD’s School of Medicine always wanted to work on gene therapy.
»Many genetic diseases are so profound and debilitating, and often, children die from them. Drugs will never be able to replace genes, so I really believe that gene therapy is the future of medicine for these kinds of disorders,« Cherqui remarks.
The path to success in the field wasn’t easy. In 2000, during Cherqui’s PhD research at Necker Hospital in Paris, many scientists still doubted if gene therapy would ever become a reality:
»It was considered as science fiction for the longest time. Many said gene therapy was so risky, it could never be used in humans,« she recalls.
Yet as 2022 drew to a close, Cherqui and her group at UCSD received a USD 4.8M grant to develop a novel CRISPR therapy for an incurable disease. The grant, provided by the Californian Institute of Regenerative Medicine (CIRM), will allow Cherqui and her team to continue their groundbreaking work using CRISPR-Cas9 technology to correct a mutated gene that causes Friedreich’s ataxia (FRDA).
FRDA: A fatal disease with no treatment
Cherqui’s former postdoc, Dr. Celine Rocca, spoke to CMN about the lab’s work on FRDA back in 2021. A multisystemic neurodegenerative disorder, FRDA is considered a rare disease, affecting one in 50,000 Americans.
FRDA is an autosomal recessive disease caused by loss-of-function mutations in the FXN gene, which encodes the mitochondrial protein frataxin. Frataxin plays roles in several key processes in iron metabolism, antioxidant protection, and energy production in the mitochondria.
The first intron of FXN bears a GAA trinucleotide repeat, which is usually between five and 30 repeats long in healthy people. Having a hyperexpansion of these repeats, however, leads to loss of frataxin production, which results in the accumulation of iron in the mitochondria and subsequent oxidative stress. FRDA patients typically have between 44 and 1700 repeats.
With no effective treatments, patients with this condition experience progressive loss of motor skills and degeneration of muscle tissue and sensory nerve fibres throughout the body, eventually resulting in the inability to walk. The majority of FRDA patients die before the age of 40.
Harnessing the therapeutic power of HSPCs
Cherqui’s novel treatment for FRDA is an ex vivo gene-edited autologous cell therapy. The process begins with extracting haematopoietic stem and progenitor cells (HSPCs) from the peripheral blood of patients before excising the trinucleotide repeat hyperexpansion in intron 1 of the FXN gene from the cells.
This edit involves delivering a ribonucleoprotein (RNP) complex consisting of Cas9 and two sgRNAs – one guide for either end of the trinucleotide expansion. In their original proof-of-concept study, the team were able to achieve editing efficiencies of more than 50% in the HSPCs of FRDA patients. Edited HSPCs display restored expression of frataxin and mitochondrial function, and can be transplanted back to patients as a one-time, curative therapy.
»Because this mutation is located within an intron in the FXN gene, it is a good target for gene correction by removing this expansion using CRISPR-Cas9. In addition, this approach would be valid for all FRDA patients, because they all carry a trinucleotide expansion mutation,« Cherqui elaborates.
Edited HSPCs are currently used for the treatment of blood disorders such as sickle cell disease and β-thalassemia. However, Cherqui’s work is novel because it offers proof that these cells can be used to treat conditions like FRDA. Edited HSPCs are able to proliferate and differentiate into macrophages and microglia in vivo in mice, and traffic to the necessary tissues throughout the body and brain of FRDA patients.
The early data shows that transplantation of the corrected HSPCs in mice prevents disease progression. The therapy will be aimed at the treatment of babies and children in whom the disease has not yet caused significant damage, however, Cherqui says they may also be able to halt disease progression in adult patients.
Cherqui’s method of utilising HSPCs eliminates the need to employ viral vectors to target specific tissues in the body, a method that is widely used for in vivo gene therapies.
»When we started to do the proof-of-concept studies, our approach worked beyond our expectations. The advantage of using HSPCs is that they are capable of self-renewal, and can do the job by themselves - they know exactly where to go. They are able to traffic to the CNS, including the dorsal root ganglia, but also the heart and muscle, which are particularly affected in FRDA patients. « Cherqui explains.
While it may seem like a narrow field of research, Cherqui’s work on FRDA is relevant to many other genetic conditions, and her lab members are continually applying this depth of knowledge to create more novel gene therapies:
»We've learned so much on the mechanism of action of HSPC-mediated tissue repair that I'm applying this strategy to many different multi-systemic degenerative disorders. This is what I always tell the students - there is no rare disease, because everything you learn on one rare disease will be applicable to so many others.«
Safety studies and clinical trials
This is not Cherqui’s first time going through the ‘bench-to-bedside’ process. Her previous work on cystinosis, another rare genetic disease, has left her well-equipped to tackle the clinical development pipeline for FRDA. The cystinosis clinical trial, which also uses gene-edited HSPCs, has an impressive safety record, with no serious adverse events, as Cherqui described at several conferences in 2022. The success of the cystinosis therapy certainly inspire confidence for the upcoming FRDA trials.
»[With cystinosis] I went from finding the gene in very early studies, to developing a gene therapy approach, all the way through to clinical trial. So, I've learned a lot. Now I have a better knowledge of what needs to be done and how to do it faster,« Cherqui says.
Cherqui and her team are currently conducting pre-clinical studies in animal models for the FRDA project to determine the safety of the therapy, and they are preparing for their first INTERACT meeting with the FDA’s Office of Tissues and Advanced Therapies (OTAT), an informal meeting during which they will discuss manufacturing, safety, and other requirements for upcoming clinical studies. The team also continues to work closely with members of the Friedreich’s Ataxia Research Alliance (FARA), who have provided funding for Cherqui’s research.
»FARA have been amazing. They provide funding, resources and support to help investigators to succeed if they want to go to clinical trials, such as providing information on disease biomarkers and disease natural history. They are very supportive,« Cherqui says.
Moving a novel CRISPR therapy from proof-of-concept studies to clinical trials can take a decade or more, and the contributions of funding agencies like CIRM are invaluable, as Cherqui concludes:
»We are lucky here in California to have the California Institute of Regenerative Medicine. Without this funding, I would never be able to progress this therapy to clinical trials – these studies require a lot of money and resources. The FDA requires very extensive safety studies, then there’s the manufacturing development including large-scale cell product productions, and the clinical trials. As an academic, this is not something we can do without the kind of funding the CIRM provides.«
Rebecca Roberts is a molecular biologist and science writer/communicator based in Queensland, Australia.
To get more CRISPR Medicine News delivered to your inbox, sign up to the free weekly CMN Newsletter here.
Tags
ArticleInterviewNewsRibonucleoprotein (RNP)Friedreich’s ataxiaRare DiseaseCRISPR-Cas
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.