Catching up on CRISPR clinical trials
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...

HIV - a CRISPR first but no cure
A clinical trial in China set a milestone in 2019 as the first to report results reported of using CRISPR in a person with HIV.
The data published in The New England Journal of Medicine researchers showed safety and longterm engraftment of CRISPR gene-edited blood stem cells as a treatment for HIV. The patient was infused with donor blood stem cells that had been gene-edited with CRISPR-Cas9 to disable the CCR5 gene, coding for a protein that HIV uses to infect immune cells. The strategy sought to replicate the 'Berlin patient' who was the first person to achieve sustained HIV remission thanks to a bone-marrow transplant from a donor homozygous for the CCR5∆32 mutation.
There were no severe complications, and the CRISPR-edited cells persisted in the patient for more than 19 months. Still, the procedure only resulted in CCR5 ablation in about 5% of lymphocytes, and HIV rebound when antiretroviral therapy was stopped.
The researchers said the long persistence is the major result of the paper and noted there is a need for further refinement of the treatment. It is currently the only CRISPR gene-editing HIV clinical trial, but eight other HIV gene-editing clinical trials are registered using zinc finger nucleases to disable the CCR5 gene.
Cancer another first, safety and feasibility but no cure
2016 marked the first patient to be injected with CRISPR-Cas9 edited cells to treat aggressive lung cancer. The trial was led by oncologist Lu You at Sichuan University, China beating US researchers to become the first testing CRISPR in humans.
“this is going to trigger 'Sputnik 2.0', a biomedical duel on progress between China and the United States”
Immunotherapy pioneer Carl June called it a new 'moon race' saying to Nature »this is going to trigger 'Sputnik 2.0', a biomedical duel on progress between China and the United States«.
June led a similar US-based cancer trial, and in 2020 reported the first peer-reviewed results from three patients with multiple myeloma and sarcoma. The Chinese study followed just two months later by reporting results involving 22 patients.
Both studies followed a strategy where immune cells are harvested from the patients and edited before being infused back into the patients. And both studies used CRISPR to disrupt the PD1 gene as a genetic approach to immunotherapy. The PD1 protein functions as a safety switch on the surface of T cells that cells can flip to stop the T cell from destroying them, and many cancer cells exploit this to evade the immune response. The US study also disrupted the T cell receptor (TCR) and added an engineered TCR that recognises an antigen expressed by cancer cells.
Both studies were safety and feasibility studies and reported that CRISPR works without severe adverse effects. As such, the studies were encouraging, to the field, though the benefit to the patients was limited.
Since the trials began, the tools have developed rapidly to improve the efficiency of editing, potentially improving the treatment.
Currently, 18 gene-editing cancer clinical trials are registered, and 10 are based in China.
Success! Sickle cell anaemia and β-thalassaemia
June 2020 saw the most successful results so far from two closely related CRISPR gene-editing trials to treat severe haemoglobinopathies - transfusion-dependent sickle cell disease and β-thalassaemia. The CRISPR-Cas9 treatment called CTX001 is developed in a collaboration between Vertex Pharmaceuticals and CRISPR Therapeutics.
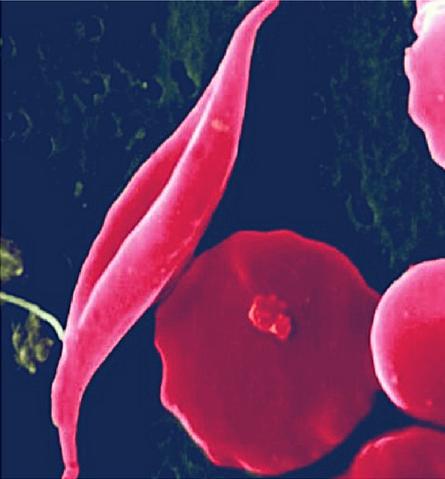
One sickle cell anaemia patient and two β-thalassaemia patients, respectively, had their blood stem cells harvested and edited with CRISPR to increase the production of fetal haemoglobin before the cells were infused back into the patients.
The edited cells had successfully populated the bone marrow and started producing healthy red blood cells in all three patients. They all reached healthy levels of haemoglobin and no longer needed blood transfusions - up to 15 months after treatment. The sickle patient also remained free of the painful complications known as vaso-occlusive crises (VOC), which require hospitalisation.
Though the patients experienced severe adverse events during the treatment, none were attributed to the CRISPR therapy.The trials have recruited four more patients whose edited cells also have populated the bone marrow successfully and started producing blood cells.
Both trials will recruit up to 45 patients, so it's still early days, but the results so far are unprecedented and support the dream of the CRISPR therapy as a one-time functional cure. As such, it may very well pave the way for treat other hard to treat heritable diseases.
Currently, four gene-editing therapies to treat severe haemoglobinopathies are in a clinical trial, two use CRISPR and two use zinc finger nucleases.
Blindness - first in vivo
In march 2020 another CRISPR milestone was widely reported in the media: The first CRISPR gene-editing treatment inserted directly in a person. The pharmaceutical companies Editas Medicine and Allergan have developed the CRISPR-Cas9 treatment for the genetic disorder Leber congenital amaurosis 10 (LCA10), which can cause blindness. As reported by Nature, the researchers will inject a virus containing the CRISPR tools directly into the eye to edit the photoreceptor cells. The CRISPR therapy called EDIT-101 works by removing the aberrant splice donor created by the disease-causing mutation in the gene CEP290. With the hope of restoring normal CEP290 expression and reactivating the photo-sensing cells.
Like the first HIV and Cancer CRISPR trials, it is a safety and feasibility study, but if there are improvements to sight, the results could be reported already this year.
It is currently the only gene-editing treatment for blindness in a clinical trial, but if successful it would be a landmark moment for the entire gene-editing field, that would likely pave the way for future in vivo trials.
Tags
ArticleCancerHuman Immunodeficiency Virus Infection, HIVSickle Cell Disease, SCDTransfusion-Dependent Beta Thalassemia, TDTCRISPR-CasZFN - Zinc finger nucleasesTrialsClinical
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.







