CRISPR Enhances CAR T-Cell Cancer Therapies
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
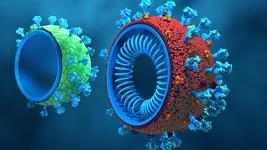
By precisely deleting the CD5 gene, which inhibits T-cell activation, American researchers have created chimeric antigen receptor (CAR) T-cells with superior antitumor activity, expansion, and persistence. This CRISPR-based gene editing was pivotal in boosting the therapeutic performance against various cancer models, including T-cell lymphomas, acute lymphoblastic leukaemia, B-cell malignancies, and solid tumours.
CRISPR-Cas9 was utilised to knock out CD5 by designing guide RNAs (gRNAs) targeting the CD5 gene. Primary T-cells were electroporated with the Cas9-gRNA complex, ensuring precise cleavage of the CD5 locus. Following successful knockout, these T-cells were further engineered to express CARs.
The knockout of CD5 was confirmed to be efficient, with more than 90% reduction in CD5 protein levels. This precise gene editing approach allowed for the creation of T-cells with enhanced therapeutic properties.
In preclinical models, CD5 KO CAR T-cells showed enhanced cytotoxicity, increased proliferation, and greater survival benefits. The deletion of CD5 was also associated with reduced exhaustion markers in T-cells, indicating a more robust and long-lasting immune response. Mechanistically, CD5 KO led to increased activation of signalling pathways critical for T-cell function, such as the Ras/ERK and PI3K/AKT/mTOR pathways.
The study provides compelling evidence that targeting CD5 can significantly improve the performance of CAR T-cell therapies, potentially overcoming some of the limitations seen in current treatments.
This research was led by Ruchi Patel and Marco Ruella from the University of Pennsylvania, and it was published on 19 July 2024 in Science Immunology.
To get more CRISPR Medicine News delivered to your inbox, sign up to the free weekly CMN Newsletter here.
Tags
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.