The Future of AAV-Delivered Gene Therapy - Engineered Capsids, Increased Potency, and Throwing Out the Rule Book
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...

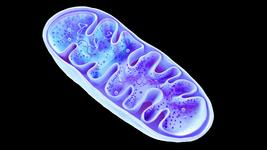
Adeno-associated viruses (AAVs) are highly useful delivery vehicles for CRISPR-Cas9 editing components. While they have several key advantages over other delivery technologies, there are several issues associated with their use, resulting in bottlenecks to greater AAV progress and the significant expense of currently available AAV-based gene therapies.
Assistant Professor Nicole Paulk, from the University of California San Francisco, is a pioneer in the field of viral gene therapy. Her laboratory at UCSF engineers disruptive technologies for AAVs, aiming to make them safer, cheaper, and more effective vehicles for gene delivery. For Paulk, getting safe and effective gene therapies to patients who need them most is the driving force motivating the lab.
Increased Potency and Stability Will Enable Low-Dose AAV
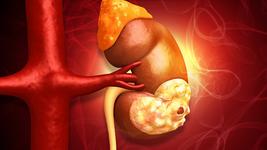
One of the issues associated with high-dose AAV gene therapy is the fact that, regardless of the target tissue or organ, the majority of systemically administered AAVs end up in the liver. Patients with pre-existing liver inflammation or disease are therefore potentially at higher risk of adverse events.
This was the case for several patients in the 2020 ASPIRO clinical trial for X-linked myotubular myopathy (XLMTM), with devastating consequences. Three patients in the trial died due to bacterial infection and sepsis following treatment, all of whom had pre-existing hepatobiliary disease. It was these tragic circumstances which prompted Paulk to write the opinion piece Gene Therapy: It’s Time to Talk About High-Dose AAV, published in Genetic Engineering & Biotechnology News.
While many researchers and clinicians have been asking how to safely administer high-dose AAVs, Paulk insists that the research community should instead be focusing on how to design AAVs so that high doses are no longer necessary. One path forward in this respect is to increase the potency of AAVs, so that each individual virus is much stronger and more effective, Paulk says. There are several approaches to increase the potency and stability of AAVs, and most are focused on altering aspects of the manufacturing and purification process and improving the reagents the vector is stored in.
Additionally, many groups are studying novel methods of administration to avoid the liver and the immune system, Paulk adds. Current intravenous systemic administration uses the veins of the hand or elbow, however other possibilities exist, including: intravenous administration from other entry points, some of which may be better suited for targeting certain tissues; utilizing infusion devices that can restrict AAVs to certain locations; direct infusions into solid organs; or infusions into other fluid compartments, like cerebrospinal fluid.
Engineering Capsids and Going Stealth Mode
Of course, the body’s immune response is a significant hurdle for administration of any gene therapy. Clinicians currently deal with this issue by treating patients with corticosteroids to temporarily blunt the immune system and prevent it from attacking the AAVs. A key area of AAV research is to engineer the capsid – the protein shell that encapsulates the virus - allowing it to more effectively reach the target cell without immune interference.
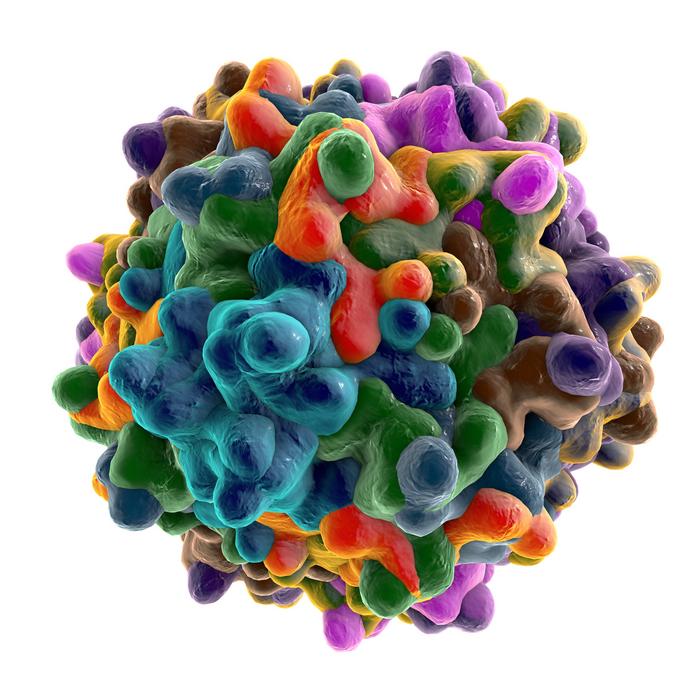
»There’s a lot of work being done with capsids. Coming up with new capsid serotypes that are either more specific for one tissue over another, or which aren’t necessarily different in their specificity compared to the ones we already have, but which are more immune-evasive. If we can engineer the capsids to be immune-evasive, they’re less likely to be bound up by either immune cells or by pre-existing neutralizing antibodies that exist in your bloodstream. This means that in a sense, they can become invisible, and are more likely to actually get to the target tissue. This is a common goal among numerous capsid engineering companies and academic labs alike,« Paulk says.
Yet another approach to this problem is to coat the AAV in a substance that will shield it from the immune response directly. »There are also groups who are trying to envelop the AAV inside other materials – things like nanoparticles, cells, viral-like particles (VLPs), lipid carriers, and exosomes,«Paulk explains.
Repurposing Bacterial Enzymes: Buying Time for AAV Delivery
Many patients are currently unable to participate in AAV gene therapy clinical trials because they have pre-existing neutralizing antibodies against AAV capsids in their bloodstream due to prior exposure to wild-type viruses. These antibodies render the treatment ineffective by inactivating the AAV before it can reach the target tissue.
An emerging method to address this issue is to re-purpose enzymes initially discovered in bacteria to eliminate pre-existing anti-AAV neutralizing antibodies in the bloodstream, and this is an area of research that Paulk is intrigued by. Engineered IdeS (immunoglobulin-degrading enzyme from Streptococcus pyogenes) and IdeZ (immunoglobulin-degrading enzyme from Streptococcus equi subspecies zooepidemicus), when administered prior to gene therapy, can result in short-term removal of anti-AAV IgG antibodies, allowing AAVs time to reach target cells.
»You can put these enzymes in the blood prior to AAV treatment, to eliminate pre-existing neutralizing antibodies against AAVs, so now you have a temporary window of time in which there are no IgG antibodies circulating in the bloodstream and you can deliver the AAV to that patient, even if they’ve been previously exposed to wild-type AAVs in nature. This could allow you to treat patients that would have otherwise been excluded from a trial. Expanding patient access to therapies, particularly for life-threatening rare diseases where there may be no alternative therapies would be transformative,« Paulk remarks.
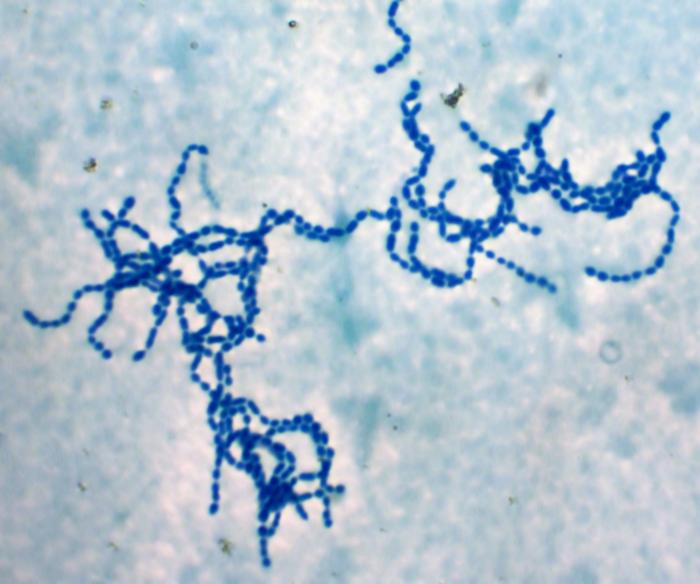
These enzymes may also offer the possibility to re-dose patients if and when necessary, Paulk explains. »Say you treated a child when they were one year old, and now they’re ten years old and their tissues have grown, and they may need to be re-dosed. You could infuse them with these enzymes that will eliminate IgG antibodies developed following their initial treatment, buying you a window of time where you can re-dose them. In a short time their normal circulating antibodies will come back, but you’ve had the chance to safely redose your patient.«
This research is still in its early stages, Paulk cautions, but it’s very promising. »These enzymes are bacterial – so, much like CRISPR-Cas9, they’re immunogenic proteins. The field is trying to find other less immunogenic orthologs or to engineer them to make them less immunogenic, so that you can deliver them into the bloodstream and not cause the body to reject them. It’s very exciting – they’ve done this successfully in primates, so it’s close, not quite ready for prime time yet, but tantalizingly close.«
Low Editing Efficiencies: Not Just an AAV Problem
Low editing efficiency is also a challenge for researchers, particularly in vivo. Paulk says AAV gene editing is often performed in the liver, because it’s the easiest target, and this typically results in around 0.1 – 1.0% of transduced hepatocytes possessing the desired functional edit. Studying and increasing editing efficiencies with AAVs is something Paulk and an enormous number of global researchers are currently working on. In the meantime, she says, one avenue for progress is to develop gene editing therapies for diseases that can be treated without the requirement for high editing efficiency.
»If you pick a disease that has positive selection – so if a cell gets corrected it will outcompete its mutated neighbours because it has a positive selective advantage – then 0.1% is more than enough, because you only need a small number of cells to have been corrected that will grow and outcompete the others. Often, we pick these simpler indications first to allow us to optimize other aspects of the process while simultaneously working to improve editing efficiency in parallel. It’s still early days but I expect, and am seeing, a lot on innovation in the near term,«Paulk remarks.
The Inverted Terminal Repeat Issue
Those familiar with AAVs will be aware that they possess rather unique genomes. AAVs have single-stranded linear DNA genomes, which is quite rare. The ends of the single-stranded genome are ‘capped’ by small structures known as inverted terminal repeats (ITRs). ITRs form where the ends of the viral DNA loop in on each other, creating the only double-stranded regions of the genome. When delivered for gene therapy, the ITRs are then bound by enzymes in the host nucleus to extend, transcribe, and translate the viral DNA. The process seems elegant and simple, however, as Paulk explains, it doesn’t always work that way.
»The problem is that ITRs are very unstable. At least, this is the case for recombinant AAVs we use in therapies, it may not be the case for wild-type AAVs. ITRs can recombine with each other and lop out everything that’s between them, and they can rearrange internally, so that your host enzymes have a hard time finding their binding recognition sequence in order to extend the genomes from single to double-stranded. They can also develop mutations such that key binding sites are now lost entirely. They’re highly mutagenic and highly unstable in this context.«
This is another key area of AAV research in which Paulk is eagerly awaiting progress from the field. »We need to come up with either new ways of making AAVs that keep the same ITR sequence but design ways to make them more stable during production, or we need to keep the same production methods but engineer new and different sequences, shapes, or orientations of ITRs that are much less likely to be recombined and mutate and become unstable. There are a number of academic groups working on this, and it’s one of the “under the radar” topics I’m hopeful for,« Paulk notes.
High Risk, Big Reward
There are many avenues forward with AAV research, many of which involve improving existing technologies that were designed for completely different problems and have been available for decades. But Paulk is an innovator; for her, sometimes the best way forward is to completely buck the trends, start from scratch, and think outside the box.
“The bigger and crazier ideas, the ones that might lead to 1000x improvements in these types of things, are the ones where we throw out the rule book entirely”Nicole Paulk
»The bigger and crazier ideas, the ones that might lead to 1000x improvements in these types of things, are the ones where we throw out the rule book entirely. Forget everything you already know about how to make AAVs. Instead of adapting techniques that were meant for monoclonal antibodies, which is what we’ve done up to this point, design something completely different. Pretend you’re an engineer and you don’t even know what a virus is. Someone comes to you and says they want an icosahedral protein with some DNA in it - how would you make it? We need to come up with entirely new ways of making AAV that are meant for, and optimized for, AAVs, instead of just adapted technologies,« Paulk elaborates.
These risky ventures, she says, have the potential to completely revolutionize the AAV field. »Those are going to be much more challenging and much less likely to work, but if they do, that could lead to the huge improvements that allow us to bring doses, costs and development times down to enable us to treat currently unreachable indications, things like diabetes and hypertension, not to mention treating patients in developing nations. The time to take these risks is now.«
Rebecca Roberts is a molecular biologist and science writer/communicator based in Queensland, Australia.
Upcoming CMN Webinar - CRISPR Delivery Systems, May 26th 2021
Tags
ArticleInsightInterviewNewsDeliveryAdeno-associated virus (AAV)
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.