Using CRISPR to cure severe hereditary immunodeficiences. Interview: Rasmus O. Bak
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
(Interview is condensed and edited for clarity)

- Tell us about the new PASCAL-MID center?
The idea behind the new center is that we have the whole workflow here in Aarhus. We have medical doctors who work on identifying novel immunodeficiencies that we in our lab can develop CRISPR reagents to correct. And then, take this back to the hospitals' transplantation unit taking care of the transplants for patients with these diseases, and do the gene-editing at clinical scale for patients.
The frame of the project is that within the 5 years, we should be ready to file for a clinical trial application and to initiate the first trials on year 6 or 7.
- what diseases do You focus on?
We have a few. There are more than 300 primary immunodeficiencies, but we need to pick a few that are relevant in terms of patients we could potentially recruit, prevalence and severity - some are not severe enough to risk the procedure of taking out the bone marrow, do the gene-editing and putting it back in.
- and what would be an example of a disease?
One of the diseases is Hyper IgE syndrome (HIES), which is a very devastating disease because patients get a lot of opportunistic infections. They have to be treated with antibiotics throughout their life.
Hyper Immunoglobulin E Syndrome (HIES)
HIES is a rare primary immunodeficiency characterized by recurrent eczema, skin abscesses, lung infections, eosinophilia, and high serum levels of immunoglobulin E, IgE, antibody. The autosomal dominant form that results mostly from mutations in the gene that encodes the transcription factor STAT3. Read more at NIH.
Monogenic disease is not just one mutation
- And I suppose it is a monogenic disease?
Well, it's a little tricky. With HIES there are different genes in which a mutation will create more or less the same disease, and we are focused on one gene called STAT3.
Another complicating factor is that not all patients have the same mutation. Unlike sickle cell disease where it's always the same mutation - a single base being substituted - for STAT3 in HIES patients, the mutations are scattered throughout the gene.
And actually, these are considerations you would have in a lot of diseases because most heritable diseases are not like sickle cell disease.
- so you have to develop a genome editing strategy for each mutation or?
Well, you could do that, but that would be a lot of work and not be a viable approach.
We are looking into hot spot regions where mutations can occur, and we try to develop a semi-universal strategy to at least fix all mutations within that hot spot. That would be more feasible.
Then we are also looking into a single universal strategy to cure most if not all of the patients.
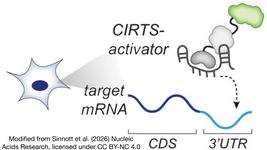
The trick is to target non-coding introns
- So to do that, you would replace part of the gene instead of correcting mutations?
Yes, you replace a larger part of the gene. And the way we are trying to do that is to target an intron - so non-coding sequences. With this strategy, if we get CRISPR-induced mutations occurring - and you can't avoid these mutations - they will not be in the reading frame of the gene.
- and how will it then correct the mutation in the exon, the coding sequence?
Yes, that's where we have to do some tricks. The CRISPR system can do knock-ins or knock-outs, and we are interested in the knock-ins either replacing part of the gene or adding in the full copy of the gene.
It is a little complicated, but the CRISPR system basically copy-pastes from a DNA template, and we can insert part of a gene like a new exon into an intron. And we can control that so the exon that we knock-in to the intron will be used instead of the mutated exon downstream.
- because you add some splicing signals?
Yes, we can add splicing signals in the exon that we integrate, and then we will splice into that exon instead of one of the other exons that carry the gene mutation. We could also fuse new exons to an existing and thereby bypass splicing. It gets a little specific on the technical side.
Rasmus O. Bak
Rasmus O. Bak heads a research group at Aarhus University, Denmark, where he is in charge of developing new CRISPR/Cas9-based technologies for gene editing and genetic engineering of blood cells, and applying these tools as gene therapies. He is well-known in the field for developing chemically modified guide RNAs, for gene editing primary human hematopoietic stem cells, and using that platform to develop a potent CRISPR/Cas9-based genome editing strategy for Sickle Cell Disease. These studies are published in highly cited papers in Nature and Nature Biotechnology.
Still early days
- That's great, and how far are you?
These are still early days. We have identified guide RNAs that are potent towards these genes, and we have different diseases and different genes other than HIES and the STAT3 gene.
But in the next month or two, we should be able to make these integration approaches where we knock-in the gene fragment.
Then, of course, there is validation - do we get a functional expression of the full gene? Do we have off-target effects? And do we maintain the stem cell properties?
- stem cell properties?
One major challenge with stem cells is to perform the whole process while the cells are in culture in the incubator without taking their unique properties away from them. So we must validate if the cells are still able to go back to the bone marrow and repopulate the blood with red and white blood cells.
It's a crucial parameter, and without that, we won't have a cure.
Safety concerns: Off-targets
- what about safety, what is the biggest concern?
The main point that people bring up is the unintended off-target activity of the CRISPR system. And of course, there will be an individual assessment of each guide RNA, because each will have its specificity profile. But honestly, until we have the first clinical trials in humans and do all the analysis, we won't know the real impact of these.
- Will it be possible to get around off-targets?
Well, we can definitely minimize them with careful design, but for most diseases, I think it will be very difficult to get rid of off-target effects completely.
You have to remember that in hematopoietic stem cells, you are dealing with a cell product with several hundreds of millions of cells, and we have a problem in detecting the off-targets mutations.
- ok?
We can do an off-target analysis. But the limit of detection is around 1 per 1,000, and if we have one cell among 500 million cells that carry a mutation, we can't detect that.
In the end, you need a very long follow-up of these patients to assess safety.
Exciting times for CRISPR and cell therapies
- Ok great, it will be fascinating to follow. Taking a broader view of the field, what do You think?
It is a very exciting time right now, and it will be very exciting to see what will happen with CRISPR therapies and gene therapies and cellular therapies within the next years.
Less than a month ago, one of the big CRISPR companies, CRISPR Therapeutics, reported their first two patients treated in clinical trials for sickle cell disease and beta thalassemia, and it seems to be working very nicely so far.
In the next couple of years there are going to be more clinical trial data coming out, and we will be able to apply these tools more broadly. For example, we will see many efforts in applying CRISPR-based therapies beyond gene correction, for example in cancer immunotherapy, regenerative medicine, and to treat autoimmune diseases.
So the next couple of years will be fascinating.
- excellent thank You very much
Center PASCAL-MID
PASCAL-MID: Personalized Approach to Genome Editing of StemCells for Autotransplantation of Monogenic Immunodeficiencies.
PASCAL-MID is a newly established CRISPR/Cas9 research center at Aarhus University, Denmark. The purpose is to develop new treatments for primary immunodeficiencies (rare monogenic disorders) by correcting genetic defects in hematopoietic stem cells.
The 'brickless' center combines experience from medical doctors and researchers to be able to offer CRISPR/Cas-based gene therapies as a standard treatment option in Denmark.
Besides Rasmus O. Bak the other PIs are Professor Peter Hokland, professor Trine Mogensen, clinical professor Bjarne K. Møller, and professor Jacob Giehm Mikkelsen.
Tags
ArticleInsightInterviewPrimary Immunodeficiency Disease, PIDGene therapyCas9
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.