Clinical Roundup: Gene-Edited Therapies for Beta Thalassemia
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
Beta thalassemia belongs to a group of incurable genetic diseases known as the thalassemias, which are characterised by adult haemoglobin deficiency. Disinct from adult haemoglobin, foetal haemoglobin (HbF) is highly expressed and critical during foetal development, and is rapidly suppressed in most individuals early in life.
HbF has been the subject of decades of intense research, and thanks to genome engineering it has become possible to switch HbF expression back on by interfering with its regulators. Reactivation of HbF expression has emerged as an attractive and popular strategy to treat beta thalassemia and related haemoglobinopathies by compensating for the lack of functional adult haemoglobin. You may read more about beta thalassemia and other genetic diseases of interest in our disease overview.
This roundup summarises the ongong clinical trials of gene-edited therapies for beta thalassemia.
Exa-cel — a CRISPR-edited blood stem cell therapy (Vertex Pharmaceuticals, Phase 3)
Exagamglogene autotemcel (exa-cel, formerly known as CTX001) is the most clinically-advanced gene-edited therapy for beta thalassemia (BT) and the related haemoglobinopathy sickle cell disease (SCD).
Exa-cel is being developed by Vertex Pharmaceuticals and CRISPR Therapeutics as an autologous, ex vivo CRISPR-Cas9 gene-edited haematopoeitic stem and progenitor cell (HSPC) therapy, with trials ongoing for both transfusion-dependant BT (TDT) and SCD.
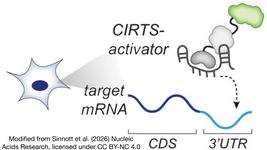
To generate exa-cel, patient-derived HSPCs are genome-edited using CRISPR-Cas9 to make a small deletion in the BCL11A gene. BCL11A (or BAF Chromatin Remodeling Complex Subunit BCL11A) is a potent repressor of HbF expression and its disruption thus leads to reactivation of HbF in the edited cells.
Exa-cel is being evaluated in the CLIMB-Thal-111 (Phase 2/3) trial for TDT. The most recent clinical data for exa-cel presented at the Annual European Hematology Association (EHA) Congress in June 2023 revealed that the trial met primary and key secondary endpoints at pre-specified interim analyses. These analyses evaluated the efficacy and safety of exa-cel in TDT patients in an ongoing Phase 3 trial as well as in the long-term follow up trial CLIMB-131. The data shared were from 48 patients with TDT dosed with exa-cel with follow-up up to 43.7 months. All patients treated with exa-cel demonstrated clinical benefit, and the mean proportion of edited BCL11A alleles was stable over time in bone marrow and peripheral blood, indicating successful permanent editing in the long-term HPSCs.
In April 2023, Vertex and CRISPR Therapeutics announced that they had completed the rolling submission of biologics licence applications (BLAs) to the FDA, marking an important milestone towards potential FDA approval of exa-cel to treat TDT and SCD.
Vertex Pharmaceuticals is also sponsoring a Phase 3 single-dose, open-label trial in paediatric participants with TDT, in collaboration with CRISPR Therapeutics. This trial, which is currently recruiting 15 participants, is expected to be completed in May 2026.
Exa-cel has already been granted multiple special designations for the treatment of TDT and SCD. The FDA has granted regenerative medicine advanced therapy, orphan drug, fast track, and rare paediatric disease designations, while the European Medicines Agency has granted a priority medicines (PRIME) designation.
EDIT-301 — a CRISPR-Cas12a-edited cell therapy (Editas Medicine, Phase 1/2)
In June 2023, Editas Medicine reported positive initial safety and efficacy data from the first TDT patient treated with EDIT-301 in the ongoing EdiTHAL Phase 1/2 trial.
EDIT-301 is an autologous CRISPR-edited cell therapy candidate, which is designed to be a one-time treatment for BT (and SCD). It works by reactivating HbF production, thereby compensating for the lack of functional adult haemoglobin in individuals with SCD and BT.
In the EdiTHAL trial, the first patient treated with EDIT-301 demonstrated successful neutrophil and platelet engraftment, and the treatment was reportedly well-tolerated, with a safety profile consistent with myeloablative conditioning with busulfan and autologous haematopoietic stem cell transplant. Editas reported that no serious adverse events occurred after EDIT-301 infusion, and that no adverse events reported were related to treatment with EDIT-301.
Specifically, EDIT-301 is developed using a CRISPR-Cas12a ribonucleoprotein to enhance the HBG1/2 promoter region in the beta-globin locus of patient-derived HPSCs. Naturally-occurring HbF-inducing mutations at the HBG1/2 region support the clinical relevance of using gene editing to enhance the HBG1/2 promoter, and this strategy has been shown to increase the red blood cell levels of HbF.
ET-01 — a CRISPR-edited blood stem cell therapy (EdiGene, Phase 1)
EdiGene, a global biotechnology company with offices in China and the U.S., is developing ET-01, an ex vivo autologous HSPC therapy that is gene-edited with CRISPR-Cas9 to express HbF.
Specifically, HbF is reactivated in ET-01 cells by disruption of the BCL11A-erythroid enhancer in patient-derived HSPCs. Besides its role in regulating HbF, BCL11A is also heavily involved in B lymphocyte maturation and haematopoeitic stem cell renewal. It was previously demonstrated that the erythroid enhancer present in the BCL11A gene sequence is required for BCL11A expression in erythroid but not in B-lymphoid cells. Therefore, specifically editing the BCL11A erythroid enhancer is anticipated to reactivate HbF while minimising any impact on BCL11A’s non-erythroid haematopoietic functions.
In November 2022, EdiGene announced completion of last patient dosing in a Phase 1 trial for ET-01 for TDT. EdiGene planned to enrol 8 participants in the trial (age range 12 to 35 years), which was run over multiple sites in China. Primary outcome measures include safety and efficacy parameters, and the trial is expected to be complete in June 2024. No clinical data has yet been released for ET-01.
Separately, EdiGene is collaborating with Institute of Hematology & Blood Diseases Hospital (China) to evalute ET-01 in an interventional trial for TDT. The trial, which is currently recruiting six patients between the ages of 6 and 35 years of age, will include two years of follow-up. Patients treated with ET-01 will also be asked to participate in a long-term follow-up study for efficacy and safety, up to 15 years after ET-01 infusion.
ST-400 — zinc finger nuclease-edited cell therapy (Sangamo Therapeutics, Phase 1/2)
ST-400 is an investigational autologous ex vivo cell therapy that consists of patient-derived gene-edited HSPCs. The cells are edited using Sangamo Therapeutics' zinc finger nuclease (ZFN) technology to disrupt a precise and specific sequence of the enhancer of the BCL11A gene. ST-400 is then infused back into the patient following conditioning chemotherapy.
ST-400 was evaluated in the THALES study to assess its safety and tolerability in adults with TDT between the ages of 18 and 40 years of age. The primary objective was to understand the safety and tolerability of ST-400. Secondary objectives include assessments of HbF levels and transfusion requirements.
At the time of the American Hematology Society (ASH) Annual meeting in 2019, ST-400 had been manufactured for five patients (18-36 years of age), three of whom had been treated by that time. Preliminary data presented at that meeting revealed haematopoietic reconstitution and on-target indels in circulating white blood cells in the three patients who had received ST-400. In a company press release at that time, Angela Smith, MD, Associate Professor in the Division of Pediatric Blood and Marrow Transplantation at the University of Minnesota, who is also a Principal Investigator of the THALES study indicated that the full effects of the treatment may take as long as 12 to 18 months or more to manifest as is the case in other myeloablative conditioning studies of stem cell transplants for beta thalassemia patients.
In a poster presented at the American Society of Hematology Annual Meeting in 2021, Sangamo provided updated clinical data from five patients treated with ST-400. The data revealed that all five patients experienced rapid haematopoietic reconstitution following dosing with ST-400, on-target edits and increased HbF levels. However, these effects diminished over time and the company revealed that the manufacturing process resulted in a loss of the long-term HSC population in ST-400. The company also revealed that no other patients would be infused with ST-400, but that already infused patients would asked to participate in a long-term study. No further details about ST-400 or the THAMES study have since been released.
ST-400 is being developed as part of a global collaboration between Sangamo Therapeutics and Sanofi, and with the support of a grant from the California Institute for Regenerative Medicine (CIRM).
CRISPR-Cas9-mediated beta globin restoration in HSPCs (BioRay Labroatories, Phase 1/2)
BioRay Laboratories, a Shanghai-headquartered company specialised in gene- and cell-based therapies are currently sponsoring two trials for CRISPR-edited cell therapies for beta thalassemia.
The first trial is a single-center, single-arm, open-label study to determine the safety and efficacy of β-globin-restored autologous HSPCs in beta thalassemia major patients with IVS-654 phenotype. The IVS-654 phenotype refers to a C→T substitution within the second intron of the HBB gene that was previously found to be one of the most common BT alleles affected in Chinese populations.
Donor-derived HSPCs will be CRISPR-Cas9-edited to restore β-globin expression. The exact gene-editing strategy has not yet been disclosed. This study will take place in collaboration with PLA 923 Hospital in China and aims to enrol up to 12 child participants (5 to 15 years). The estimated study completion date is 1st December 2023. Each participant will receive a single dose of edited cells throughout the year-long study.
BioRay is also recruiting for a Phase 1 trial of another CRISPR-edited HSPC therapeutic candidate BRL-101. BRL-101 is an autologous cell therapy candidate in which the the BCL11A enhancer is CRISPR-edited to restore HbF expression. Up to nine participants (between the ages of 3 and 35 years old) will receive a single infusion of BRL-101, and this trial is expected to be completed in September 2026.
Primary and secondary outcome measures are similar for both trials sponsored by BioRay, and include safety and efficiency assessments at regular intervals to monitor haemoglobin levels and transfusion status. Trial participants may also be asked to participate in a subsequent long-term follow-up study that will monitor the safety and efficacy of the treatment for up to 15 years post-infusion.
CRISPR-Cas9-Edited Induced Haematopoietic Stem Cells to Treat Beta Thalassemia (Allife Medicine, Phase 1)
Allife Medical Science and Technology (China) is sponsoring an ongoing Phase 1 trial to evaluate the safety and efficacy of a CRISPR-Cas9-edited induced haematopoietic stem cell (iHSC) therapy to treat BT. The study was initated in 2019 with 12 patients between the ages of 2 and 60 years old.
In the experimental therapy, CRISPR-Cas9 is used to correct the underlying HBB mutations in patient-derived iHSCs ex vivo, and the edited cells are then transfused back into the patients. The trial is open-label single-arm meaning that all study participants will be treated identically, i.e., there is no control or comparator group. No results have yet been posted for this trial.
You can find all our previous news articles about gene-editing clinical trials here. For a complete overview of CRISPR IND approvals and ongoing gene-editing trials, check out CRISPR Medicine News' Clinical Trials Database.
This roundup was originally published on 2nd February 2022. It was updated and republished on 26th July 2023 to reflect updates to ongoing clinical trials of gene-edited therapies for beta thalassemia.
To get more of CRISPR Medicine News delivered to your inbox, sign up to the free weekly CMN Newsletter here.
Tags
ArticleNewsClinical News Updatesin vivoElectroporationBeta ThalassemiaTransfusion-Dependent Beta Thalassemia, TDTCRISPR-CasCas9EdiGene, Inc.Sangamo Therapeutics Inc.Shanghai Bangyao Biotechnology Co., Ltd. - BioRay LaboratoriesVertex Pharmaceuticals, Inc.Trials
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.