Catching up on CRISPR Delivery Methods
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...

New AAV vectors for gene therapy
Adeno-associated virus (AAV) vectors are the vehicle of choice for in vivo delivery of genetic material into cells. Because they cannot replicate without the aid of a helper virus, they are deemed safer that other viral vectors, and they are used in a number of approved therapies on the market. However, despite their advantages over other viral vectors, AAV vectors have limited cell-type selectivity and some cell types are refractory to known AAVs.
In May, we interviewed Kathleen Börner from the Department of Infectious Diseases/Virology at Heidelberg University in Germany. Börner, along with colleagues at Heidelberg University and collaborators at the University of Florida addressed the shortcomings of AAV vectors by developing a system to rapidly identify new AAV variants with specificity for desired cell types.
Börner’s area of interest is HIV, and she initially set to find new AAVs that could transduce T cells and macrophages, since these are poorly transduced by wild-type AAVs. However, the outcome exceeded all expectations.
By genetically engineering small peptides into the AAV capsid, the group generated new AAV variants that collectively had the ability to transduce more than 90 different cell types. They screened each new variant in a high-throughput assay that they also developed during the project. The assay is simple and clever. Each engineered AAV encodes a yellow fluorescent protein (YFP). Transduced cells express YFP and the level of fluorescence emitted is used to calculate transduction efficiency.
»In most instances, we found an AAV suitable for targeting the cell type our collaborators or we were interested in,« said Kathleen Börner. Remarkably, the results of the work have been available in a free and searchable online database called SPIRIT.

Using Sound Waves to Deliver Gene Therapies
If anyone knows the importance of developing better and safer ways to deliver gene therapies, it is those treating the patients most in need. In May, we caught up with Steven Jonas, a paediatric hematology oncology physician at UCLA who explained the delivery challenge very well:
»Whether we're talking about a gene editing therapy, a stem cell transplant, or a cancer immunotherapy, there's a thread that connects them together. And that is the need to deliver some kind of gene or gene editing package to many cells efficiently, quickly and cost effectively. A lot of these therapies right now are extraordinarily expensive, and take a long time to make«.
Jonas teamed up with collaborator Paul Weiss, Professor in Chemistry, Bioengineering and Materials Science at the California Nanosystems Institute at UCLA to solve the ‘one billion per hour’ criterion, that is the number of cells needed for one stem cell treatment for a young child. The team developed an acoustofluidic device that uses sound waves to create pores in cell membranes through a glass capillary. The pores permit the entry of foreign DNA, e.g., gene editing machinery without compromising cell viability. In a proof of concept experiment, the team showed that the device could process 200,000 cells per minute with confirmed expression of a plasmid-delivered reporter gene in primary haematopoietic cells.
The team has plans to advance the new delivery advice for a number of treatment strategies (gene editing, therapeutic proteins, immunotherapy) within paediatric cancer and bone marrow transplant therapies. We look forward to following the work!
Read our full interview with Steven Jonas and Paul Weiss here.

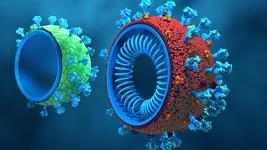
Organ-Specific CRISPR with SORT Nanoparticles
Nanoparticles are a popular and so far safe choice for the efficient delivery of CRISPR-Cas and other gene editing machinery to cells, and they are also used in the first FDA-approved siRNA therapy (Onpattro) for a rare nerve disease.
However, despite their popularity and advantages over other delivery methods, the established nanoparticle approaches do not exhibit organ or tissue specificity. In June, we interviewed Daniel Siegwart PhD, from The University of Texas Southwestern Medical Center to hear about how his team has addressed this limitation.
By supplementing established lipid nanoparticles with specialised SORT (Selective organ targeting) molecules, Siegwart’s team were able to generate modified nanoparticles whose unique biological identities direct them to specific organs and tissues in mice, including lungs, spleen, liver. SORT nanoparticles are compatible with many gene editing modalities, including CRISPR-Cas9 single guide RNA and Cas9 ribonucleoprotein complexes, and the team showed that the SORT approach could be used to knockdown a number of disease relevant genes in mice.
SORT nanoparticles are scalable and overcome the common fate of nanoparticle-based drug delivery where ‘all nanoparticles go to the liver’, opening the door for new therapies for a broad range of inherited genetic diseases and cancers. The technology has been licensed to ReCode Therapeutics for the development of new therapies for the devastating autosomal recessive lung disorders Cystic Fibrosis and Primary Ciliary Dyskinesia.
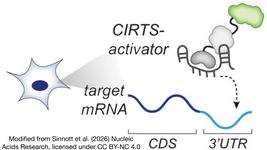
Organ-Specific In Vivo CRISPR With Cas12a Nanoclews
Viral vectors and lipid nanoparticles dominate the emerging strategies to solve the CRISPR delivery challenge. In June, we spoke to researchers from the University of California, Los Angeles (UCLA) who have taken a completely different approach to CRISPR delivery.
Dr. Zhen Gu leads a group of researchers in developing bioresponsive drug delivery systems that deploy signal-responsive materials and devices for enhanced control of drug delivery. In his former lab at the University of North Carolina he led the development of a novel prototype for in vitro delivery of CRISPR reagents. This was based on a so-called DNA nanoclew, a spherical core of DNA onto which CRISPR-Cas9 reagents and other materials can be added in layers, resulting in an assembly that can traverse the cell membrane to reach the nuclease without compromising cell viability.
Gu’s lab has now taken the DNA nanoclew a step further, and shown that it can be used to deliver CRISPR gene editing reagents in vivo in an organ-specific manner. In the new work, the group used Cas12a endonuclease, which is smaller than and is less prone to off-target editing than Cas9. The researchers built a gene editing assembly layer-by-layer and directed it to hepatocytes by conjugating galactose, which is a known hepatocyte ligand.
»Our system is a ‘smart’ one that can change its surface charge depending on the physiological environment. It’s also composed of biocompatible materials that can be easily synthesised without the generation of environmental hazards. Its biodegradability reduces the concern for long-term nanomaterial accumulation in the body. Ultimately, we see our DNA-based carrier as a platform system, where the binding sequence can easily be adjusted to deliver different CRISPR tools«, said Zhen Gu about the work.
Safety Considerations Around Delivery
As CRISPR edges closer to the clinic with a number of exciting clinical trials underway, safety remains a concern. Worries about off-target edits that may result in heritable genetic changes, unwanted immune responses to CRISPR reagents, and potentially cancer-causing p53-mediated responses to CRISPR-induced double strand DNA breaks are among the major concerns within the field.
In two separate interviews conducted late last year, we discussed safety concerns around CRISPR with Roberto Nitsch, Associate Director in Clinical Pharmacology and Safety at AstraZeneca and Bence György,head of the clinical translational research group at the Institute of Molecular and Clinical Ophtamology Basel (IOB), Switzerland.
Robert Nitsch took us through the safety considerations that arise when trying to advance a gene editing technology from research to the clinic in less than 10 years. Bence György discussed specifically the risks associated with using AAVs for CRISPR delivery.
Although it is critical to maintain discussions around the safety of CRISPR gene editing and delivery, it is also very promising to see that the first CRISPR clinical trials show that CRISPR not only works but seems safe. For more on this, you can read our recent coverage of the first CRISPR clinical trials results.
Tags
ArticleDeliveryIn vivoAcoustofluidicsDNA nanoclewsLipid-based nanoparticleAdeno-associated virus (AAV)Gene therapyCRISPR-CasSafety
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.