Disease Roundup: Four Gene-Editing Candidates in the Clinic for Sickle Cell Disease
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
The original version of this article was published on 30th December 2021. It was updated and republished on 20th September 2023 to reflect further clinical developments in the CRISPR medicine field for sickle cell disease.
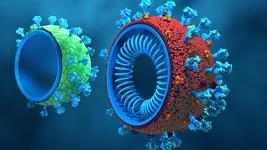
Sickle cell disease (SCD) is a group of diseases that are characterised by defective adult haemoglobin, which belong to a larger family of autosomal-recessive blood disorders known as the haemoglobinopathies (See Fact Box).
A number of treatments exist to manage the symptoms and complications of SCD but none of these are curative. Hydroxyurea was the first medication to obtain FDA approval for SCD (1997). It is an anti-cancer agent that promotes the production of foetal haemoglobin by a poorly understood mechanism and is widely used today despite side effects. Other treatments include Endari (2017), which increases L-glutamine levels in the blood triggering a cascade of events that reduces oxidative stress in sickled cells, allowing them to retain some function, Oxbryta (2019), which prevents defective haemoglobin from aggregating, thus ameriolating the symptoms of SCD, and Adakveo (2019), a monoclonal antibody that blocks P-selectin, thus lessening the inflammation associated with SCD.
Gene editing provides new hopes for SCD patients
Fortunately for the millions of SCD sufferers worldwide, decades of research to unravel the genetic pathways involved in regulating haemoglobin production has opened doors for diverse gene-editing approaches that aim to cure the disease.
There are currently four clinical-stage candidates in development, three of which aim to restore foetal haemoglobin (HbF) expression through gene editing of patient-derived cells, and a single candidate that aims to tackle the root cause of SCD by direcly correcting the disease-causing mutation in patients' own cells.
1. Exa-cel: Vertex Pharmaceuticals and CRISPR Therapeutics (Phase 3)
Exa-cel (formerly known as CTX001) is the most clinically-advanced gene-editing therapeutic candidate worldwide. It is co-developed by Vertex Pharmaceuticals and CRISPR Therapeutics as a single-dose curative treatment for severe sickle cell disease (SCD) and the related disease blood transfusion-dependent beta-thalassemia (TDT).
Specifically, CRISPR-Cas9 is used to disrupt the BCL11A gene in a patient’s own haematopoietic stem cells (HSCs) ex vivo, and the engineered cells are then transplanted back into the patient where they express HbF to restore healthy red blood cell levels.
The ongoing CLIMB-121 (safety and efficacy in SCD) and CLIMB-111 (safety and efficacy in TDT) trials were the first ever CRISPR gene-edited therapy trials to be sponsored by US-based companies, and in June 2023, it was announced that the FDA accepted Vertex Pharmaceuticals’ biologics license application (BLA) for treating severe SCD and TDT. Similar applications were submitted in the EU and UK in 2022.
Exa-cel is anticipated to become the first ever gene-edited therapy to be approved for use in humans. The candidate is currently being evaluated in a number of clinical trials for the treatment of SCD, as follows:
- CLIMB-121, a Phase 1/2/3 open-label trial to assess the safety and efficacy of a single dose of exa-cel in patients ages 12 to 35 years with severe SCD, that is defined by having at least two severe VOCs per year in the two years before enrolment. This trial is now closed for enrolment, and participating patients will be followed for approximately two years after exa-cel infusion. Each patient will be asked to participate in the long-term follow-up (LTFU) study CLIMB-131.
- CLIMB‑151, a Phase 3 open-label trial to assess the safety and efficacy of a single dose of exa-cel in patients ages 2 to 11 years with severe SCD, that is defined by having at least two severe VOCs per year in the two years before enrolment. This trial is recruiting to enrol approximaetly 15 patients aged 5 to 11 years at sites in the UK, US and Italy, with the plan to extend to ages 2 to less than 5 years at a later date. Patients partipicating in the CLIMB-151 trial will be followed for approximately two years after infusion, and each patient will also be asked to participate in the LTFU CLIMB-131 study.
- CLIMB-161, an ongoing Phase 3b trial to support expansion of Vertex' manufacturing footprint after initial potential approval and launch of exa-cel. This trial is expected to enrol approximately 12 patients aged 12 to 35 years, with either TDT or SCD characterised by recurrent VOCs. Patients participating in CLIMB-161 will be followed for approximately one year after infusion, and will also be asked to participate in CLIMB-131.
Positive clinical data for exa-cel in the treatment of severe SCD
In June 2023, results from the CLIMB-121 trial were announced at the Annual European Hematology Association Congress. According to a press release published by Vertex at that time, of the 35 SCD patients receiving exa-cel, 17 were eligible for the evaluation of primary and key secondary endpoints at the time of analysis. 16 of these 17 patients (94.1%) had been VOC-free for at least one year, andd the mean VOC-free duration was 18.7 months, with a maximum of 36.5 months.
All 17 patients achieved the key secondary endpoint of being free from hospital stays related to VOCs for at least 12 consecutive months. The one patient who did not require hospitalisation due to VOC-related reasons was not completely VOC-free and had a complex set of comorbidities. An analysis of all SCD patients revealed the mean HbF level to account for more than 30% of total haemoglobin by the third month and was then maintained at approximately 40% through follow-up, with pancellular distribution.
In SCD patients, the increase in HbF levels occurred mostly within the first few months of therapy and was maintained. The mean proportion of edited BCL11A alleles present in bone marrow and peripheral blood was stable, indicating successful permanent editing of the long-term haemopoietic stem cells. There were no severe adverse events related to exa-cel in SCD patients.
So far, exa-cel has been granted Regenerative Medicine Advanced Therapy (RMAT), Fast Track, Orphan Drug, and Rare Pediatric Disease designations from the U.S. Food and Drug Administration (FDA) for TDT and SCD, as well as Orphan Drug Designation from the European Commission, and Priority Medicines (PRIME) designation from the European Medicines Agency (EMA), for both TDT and SCD.
2. EDIT-301: Editas Medicine (Phase 1/2)
EDIT-301 is being developed by Editas Medicine as an autologous CRISPR-edited cell therapy for the treatment of severe SCD. The candidate is being evaluated in the RUBY Phase 1/2 trial in 40 adult participants between the ages of 18 and 50 years. The single-arm, open-label, multicenter trial is actively recruiting, and the overall goal is to evaluate the efficacy, safety and tolerability of EDIT-301 in adults with severe SCD.
EDIT-301 is the first experimental medicine developed using CRISPR-Cas12a gene-editing technology, and it is specifically edited using a CRISPR-Cas12a ribonucleoprotein to enhance the HBG1/2 promoter region in the beta-globin locus of patient-derived HPSCs. Naturally-occurring HbF-inducing mutations at the HBG1/2 region support the clinical relevance of using gene editing to enhance the HBG1/2 promoter, and this strategy has been shown to increase the red blood cell levels of HbF.
In June 2023, Editas announced positive initial safety and efficacy data from the first four patients with SCD treated with EDIT-301 in the RUBY trial. Specifically, the company reported that Patients 1 and 2 reached normal haemoglobin levels five months after treatment with EDIT-301, and that both patients had maintained normal haemoglobin level at ten- and six-month follow-ups, respectively. For all patients, HbF levels of greater than 40% were also reported to persist during the same time frame. Patients 3 and 4 experienced increases in total haemoglobin and HbF at three and two months of follow up, respectively, that follow similar trajectories as those seen in the first two patients. All four treated RUBY patients were also reported as being free of VOEs since infusion.
EDIT-301 was reported as being well-tolerated, demonstrating a safety profile consistent with myeloablative conditioning with busulfan and autologous haematopoietic stem cell transplantation by the four patients in the RUBY trial, and no adverse events reported during the trial were related to treatment with EDIT-301.
EDIT-301 has been granted FDA Orphan Drug Designation for the treatment of SCD, and Rare Pediatric Disease Designation for the treatment of SCD in individuals from birth to the age of 18 years.
FACT BOX: Sickle Cell Disease and Foetal Haemoglobin
Sickle cell disease (SCD) results from a single-point mutation in the haemoglobin subunit beta (HBB) gene and is associated with a range of symptoms and life-limiting complications. Vaso-occlusive crises (VOEs or VOCs) are the most commonly encountered complication in severe SCD, and these occur when small blood vessels get blocked because of sickled red blood cells which tend to be stiffer than healthy cells, and because the defective form of haemoglobin seen in SCD (haemoglobin S) renders the red blood cell membranes sticky.
Daily treatment for SCD patients is limited to symptom control, dietary intervention and pain management. While a bone marrow transplant from a healthy matched donor has traditionally been the only (albeit slight) hope of a cure for the haemoglobinopathies, gene-editing technology unleashes the possibility to cure a patient using their own cells. Central to many of the current approaches is foetal haemoglobin (HbF).
HbF is highly expressed and critical during foetal development, but then rapidly suppressed early in life. Extensive research on the molecular mechanisms of the haemoglobinopathies revealed that the B-cell lymphoma/leukaemia 11A gene, BCL11A, is a negative regulator of HbF expression, and that its disruption could restore HbF expression and reverse SCD in mice by compensating for the lack of functional adult haemoglobin. Since the discovery of this so-called haemoglobin switch, reactivation of HbF expression has emerged as a dominating therapeutic strategy for SCD (as well as beta-thalassemia).
3. BEAM-101, Beam Therapeutics (Phase 1/2)
BEAM-101 is the first base-edited therapy candidate for a haemoglobinopathy, and is developed as a patient-specific, autologous haematopoietic stem and progenitor cell (HSPC) therapy designed as a one-time treatment for SCD and TBT.
In late 2021, Beam Therapeutics announced that the U.S. FDA had cleared BEAM-101 for clinical evaluation as a treatment for SCD.
BEAM-101 cells are engineered ex vivo with an adenine base editor (ABE) that incorporates A → G base edits in the HBG1 and HBG2 gene promoters, which regulate the expression of HbF. These edits mimic the naturally-occurring HbF-inducing mutations observed in individuals that continue to produce foetal haemoglobin beyond infancy, leading to reactivation of HbF expression to compensate for the lack of adult haemoglobin in SCD. The BEAM-101 base-editing reagents are delivered to patient-derived haemopoetitic stem cells via electroporation.
Results from animal studies reveal high levels of base editing and robust HbF induction after long-term in vivo engraftment with BEAM-101 cells.
According to a company press release published in November 2022, the first patient has been enroled in the BEACON Phase 1/2 clinical trial of BEAM-101. Recruiting is still ongoing for this trial, which aims to assess the efficacy and safety of BEAM-101 in an estimated 15 adult participants.
4. CRISPR_SCD001, University of California, U.S. (Phase 1/2)
Mark Walters, MD at University of California, San Francisco Benioff Children's Hospital Oakland, in collaboration with University of California, Los Angeles and University of California, Berkeley is sponsoring a Phase 1/2 clinical trial for severe SCD in 9 participants between the ages of 12 and 35 years old.
During the study, the participants will receive a single intravenous transfusion of CRISPR_SCD001, which is an autologous experimental therapy based on patients' own red blood cells that are CRISPR-Cas9-edited to directly correct the mutation in the beta-globin gene responsible for SCD. CRISPR reagents are delivered to the cells via ribonucleoprotein. Before transfusion, each partipicant will undergo a myeloablative conditioning procedure with the chemotherapeutic busulfan. Myeloablative conditioning destroys the cells in the bone marrow to prevent rejection of the transfused CRISPR_SCD001 therapy.
Recruitment is ongoing for this study, which is expected to enrol the first patient in June 2024. The estimated study completion date i.e. the date whereby data is available on the last study participant is set to June 2028.
BIVV003: Sanofi, France (Phase 1/2, clinical development halted)
BIVV003 (also known as SAR445136) is an ex vivo-engineered autologous HSPC therapy that was designed to express HbF through BCL11A disruption. In contrast to exa-cel, BIVV003 is edited using a zinc finger nuclease (ZFN) mRNA that, once translated, targets the BCL11A locus. BIVV003 is developed using Californian Sangamo Therapeutics' proprietary ZFN technology.
The candidate was developed as a one-time intravenous treatment for severe SCD, and is currently undergoing evaluation in the Phase 1/2 PRECIZN-1 study for severe SCD, which was initially sponsored by Sanofi. The study will evaluate its safety, tolerability, and efficacy of autologous HSPC transplantation using BIVV003 in up to 8 adult patients. Patient participation in this trial is approximately 136 weeks, and enrolled subjects will be asked to participate in a separate long-term follow-up study to monitor the safety and efficacy of BIVV003 treatment for a total of 15 years post-transplant.
In January 2022, Sangamo announced the transition of the BIVV003 (SAR445136) SCD programme from Sanofi to Sangamo. According to the same press release, the Phase 1/2 PRECIZN-1 study was expected to be completed as planned, with the final patients in the study expected to be dosed in the third quarter of 2022. Despite promising 6-month data for the first patient dosed with BIVV003 manufactured using improved methods, in a 2022 business update, Sangamo announced a strategic decision to halt further investments in the programme beyond completion of the PRECIZN-1 study, to redeploy resources to its Fabry and TX200 programmes, and to seek a potential collaboration partner to progress this asset to a potential Phase 3 trial.
We strive to keep you updated with clinical and pre-clinical news from the CRISPR Medicine field. For a complete overview of current gene editing clinical trials, check out CRISPR Medicine News' Clinical Trials Database.
To get more of the CRISPR Medicine News delivered to your inbox, sign up to the free weekly CMN Newsletter here.
Tags
ArticleClinical News Updatesin vivoRibonucleoprotein (RNP)Adeno-associated virus (AAV)Beta ThalassemiaSickle Cell Disease, SCDBlood diseaseRare DiseaseCalifornia Institute for Regenerative Medicine (CIRM)University of CaliforniaBase editorsCRISPR-CasCas12aCas9ZFN - Zinc finger nucleasesBeam Therapeutics Inc.CRISPR Therapeutics AGEditas Medicine, Inc.Graphite Bio, Inc.Intellia Therapeutics, Inc.Novartis AGSangamo Therapeutics Inc.Sanofi S.AVertex Pharmaceuticals, Inc.TrialsClinical
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.