Interview Roundup: CRISPR Approaches To Curing Rare Diseases
CMN Intelligence - The World’s Most Comprehensive Intelligence Platform for CRISPR-Genomic Medicine and Gene-Editing Clinical Development
Providing market intelligence, data infrastructure, analytics, and reporting services for the global gene-editing sector. Read more...
Correcting β-thalassemia with a single CRISPR edit
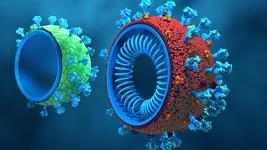
β-thalassemia (BTT) is one of the most common rare genetic diseases and arises through any of >200 loss-of-function mutations in the β-globin gene (HBB), which encodes one of the two building blocks in haemoglobin.
HBB mutations result in a shortage of mature and functional adult haemoglobin, leading to a spectrum of symptoms ranging from mild to severe anaemia and early mortality, depending on the exact mutation(s) present. Current treatments are limited to disease management and long-term prognosis is poor.
The α-globin genes (HBA1 and HBA2) produce the other building block α-globin, and in BTT, the lack of β-globin results in excess unpaired α-globin that forms red blood cell-killing aggregates to further complicate the disease.
CRISPR Therapeutics and Vertex Pharmaceuticals are making huge progress in developing their joint CTX001 candidate for BTT and the related sickle cell disease (SCD). CTX001 works by genetically reactivating foetal haemoglobin (HbF) to compensate for the lack of haemoglobin in BTT or the defective haemoglobin in SCD.
In an alternative approach to BTT, two research groups have recently replaced one of the HBA genes with a healthy full-length HBB gene in a single CRISPR edit.
Mario Amendola and his group at the non-profit research institution Genethon in France introduced the concept first in July 2020 with four rare diseases and in February 2021 the same group repeated the approach to correct β-thalassemia. Shortly after, in March 2021, Danny Dever and Matthew Porteus at Stanford University managed to do the same thing, using CRISPR-Cas9 to swop one of the HBA genes for a healthy full-length HBB gene. In both studies, gene replacement was performed in patient-derived haematopoeitic cells ex vivo, which were then transfused into mice and monitored for their long-term ability to reconstitute the haematopoeitic lineage in vivo. The strategy allowed the researchers to simultaneously downregulate α-globin and upregulate β-globin through the α-globin promoter, ensuring that the building blocks were present in a healthy balance and essentially killing two birds with one stone.
Plug-and-play expression of therapeutic transgenes in blood cells
In March, we caught up with Mario Amendola, a group leader at the non-profit research institution Genethon in France, to hear about how recent work from his group resulted in a plug-and-play transgene knock-in platform that has the potential to treat a range of rare genetic diseases.
Approximately 7,000 distinct rare genetic diseases affect around 300 million people globally. CRISPR may be the holy grail when it comes to curing genetic disease, but developing 7,000 cures is a massive scientific challenge. Mario Amendola’s goal is to find a one-size-fits-all genetic solution to that challange, and his main focus is on one group of diseases, as he told us in our interview:
»There is a group of diseases which are very different from each other, but what they all have in common is the lack of expression of a specific protein in the blood. The specific protein varies from disease to disease, but most of them can be treated in the same way by injecting the missing protein into the blood.«
Amendola had the idea that genome editing could be used to make blood cells deliver a constant supply of the missing protein, by genetically engineering the cells rather than injecting the missing protein, which sounds simple but suffers many limitations. The team developed an ex vivo CRISPR platform to express clinically relevant proteins from cells of the erythroid lineage, under the control of the α-globin promoter.
Using this new approach, which is described in more detail in the full interview, the team was able to integrate many different transgenes to the genome of human haematopoeitic stem/progenitor cells (HSPCs).
Once in place, they tested the new setup on 4 rare genetic diseases; haemophilia B (Factor IX deficiency), and Hurler syndrome, Fabry disease and Wolman disease, the latter 3 being lysosomal storage disorders characterised by deficiency in one of 3 single digestive enzymes. In all cases, expression of the missing gene from the endogenous α-globin promoter in HSPCs, through ex vivo CRISPR editing, led to marked upregulation in the corresponding mRNA transcripts and in the protein levels following differentiation of the HSPCs to erythroid cells. The concept was further tested with promising results in patient-derived cells exposed to conditioned media from transgene-expressing HPSCs, and in mice, with engraftment, erythroid cell repopulation and differentiation into HSPC lineages.
The group shared their proof-of-concept findings in a paper published in Nature Communications last summer. In a more recent publication in Blood Advances (February 2021), the same group described a similar approach to treat β-thalassemia, where they combined a knock-in with a knockout to replace one of the α-globin genes with a healthy full-length HBB gene, allowing them to balance the expression of these two essential proteins.

Reversal of β -thallassemia through full-length gene replacement
In April, we interviewed Danny Dever about his work in developing a potential cure for the haemoglobinopathy β-thalassemia.
Danny Dever is a former Research Instructor in Matthew Porteus’ lab at Stanford University, and he is a co-founder of San Francisco-based gene-editing company Graphite Bio.
In work that was published in Nature Medicine in March 2021, Danny Dever, together with Matthew Porteus, led the Porteus lab in replacing one of the HBA genes with a healthy full-length HBB gene in a single CRISPR edit as described above. Although the team could prove the concept in mice and BTT patient-derived red blood cells, the approach has yet to be translated to humans. In the envisioned setup, patients would essentially become their own donor. Replacement of a HBA gene rather than the mutated HBB gene would preserve any residual β-globin a patient may express, depending on the severity of their HBB mutations.
Defeating Friedreich's Ataxia with CRISPR
In July, we spoke with Dr. Céline Rocca from the Cherqui Lab at the University of California San Diego, to hear about her work in developing a CRISPR-based therapy for Friedreich's Ataxia (FRDA).
FRDA is a rare and incurable multisystemic neurodegenerative disorder that occurs in about 1 in 40,000 people, of which almost 60 % will die prematurely from cardiac malfunction. Treatment options are limited to managing associated health issues and prolonging the lifespan of sufferers, and most individuals are wheelchair-bound within 15 years from diagnosis.
The disease is caused by a hyperexpansion of tricnucleotide repeats (GAA) in the first intron of the FXN gene, which encodes the mitochondrial protein frataxin that plays multiple roles in metabolism and antioxidant protection in the mitochondria. The hyperexpansion impairs the function of frataxin, causing a myriad of symptoms, and disease severity and age of onset correlates directly with the number of repeats.
In 2020, Céline Rocca and colleagues made a breakthrough in FRDA when they sucessfully used CRISPR-Cas9 to remove the GAA expansions in human FRDA lymphoblasts, restoring healthy levels of frataxin expression and normalising mitochondrial activity. The team behind the work demonstrated normal haematopoiesis of CRISPR-edited cells in vitro and in vivo in immunodeficienct mice. That work was published in Molecular Therapy, and it provides the groundwork for the clinical translation of autologous transplantation of gene-corrected HSPCs for FRDA.
In our interview, Céline Rocca shared with us the significance of her work in FRDA to date, as well as the limitations in currently-available animal models to study FRDA, both from a research and therapeutic perspective. She also discusses the approaches that she and others have explored in order to obtain a more realistic picture of disease with animal models of FRDA.
Although Céline Rocca's focus has been FRDA, the lack of precision animal models that recapitulate the genetics and phenotypes of disease is a major bottlenck in the rare diseases field in general, making it difficult to fully understand disease aetiology, find viable therapeutic targets, and test new therapies.

A long road to correcting X-Linked Agammaglobulinemia
Earlier this week, we published an interview with Dr. David Gray from the Kohn Lab at the University of California, Los Angeles. This interview is a great story of resilience within research. In April of this year, having travelled a long and winding research path that began in 2015, Gray published a paper in The CRISPR Journal describing the process of editing the gene responsible for X-Linked Agammaglobulinemia (XLA), which essentially laid the groundwork for pre-clinical studies on this rare immunodeficiency.
XLA arises through a myriad of mutations in the Bruton's tyrosine kinase (BTK) gene, which result in defective B cell receptor (BCR) signalling and a deficiency in B cells. Without mature B cells, patients lack antibodies and are highly susceptible to infection.
Although affected individuals can receive regular antibody supplementation from healthy donors, there is no long-term treatment option or cure. However, since it's arrival to the gene therapy toolbox, CRISPR has become a major avenue for XLA researchers with hopes that it can cure the disease.
During our interview, David Gray told us how he and colleagues rationalised that full-length replacement of the BTK cDNA would be a reasonable strategy to cure XLA, since the disease is characterised by many mutations that are dispersed throughout the entire gene.
The project began while Gray was a PhD and although the idea sounded simple - they only had to cut the gene and add in a functional copy into its endogenous locus - the task turned out to be very challenging.
Gray spent much time optimising the efficiency of integration as well as the expression of the integrated transgene (i.e. the full length BTK). All of these optimisation steps had to be carefully considered and balanced in light of the fact that too much BTK is known to be toxic. Moreover, XLA has a moderate treatment plan - unlike many other rare diseases for which no dedicated treatment exists at all - and this needed to be factored into the benefit and risk considerations.
Another challenge was delivery; getting such a big gene (BTK is more than 3 kb long) as well as the necesssary CRISPR-editing components into an adeno-associated virus (AAV) packaging vector that has a maximum capacity of 4.7 kb is no mean feat. This led to a new round of troubleshooting where Gray and colleagues began testing various truncations of BTK as well as various guide RNAs and exogenous regulatory elements to find the setup that could edit cells with high enough efficiency that resulted in desirable levels of functional BTK protein expression.
After years of tedious and frustrating work, the Kohn Lab now has the setup in place to progress with pre-clinical studies to test a CRISPR-Cas9-based cure for XLA, and animal studies are being intitiated.
Read the full interview with David Gray here.
This catchup focused on a selection of our scientific interviews with researchers working in the CRISPR field. To catch up with the clincal developments within CRISPR medicine, you can read our clinical update articles here, and you can find a list of all CRISPR clinical trials in our CRISPR Medicine News' Clinical Trials Database.
Tags
Articlein vivoAdeno-associated virus (AAV)Beta ThalassemiaBlood DiseaseFriedreich’s ataxiaMucopolysaccharidosis I, MPS IMucopolysaccharidosis type II, MPS IIBlood diseaseRare DiseaseCRISPR-CasCas9
CLINICAL TRIALS
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.
Sponsors:
Base Therapeutics (Shanghai) Co., Ltd.